Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Medi Study Go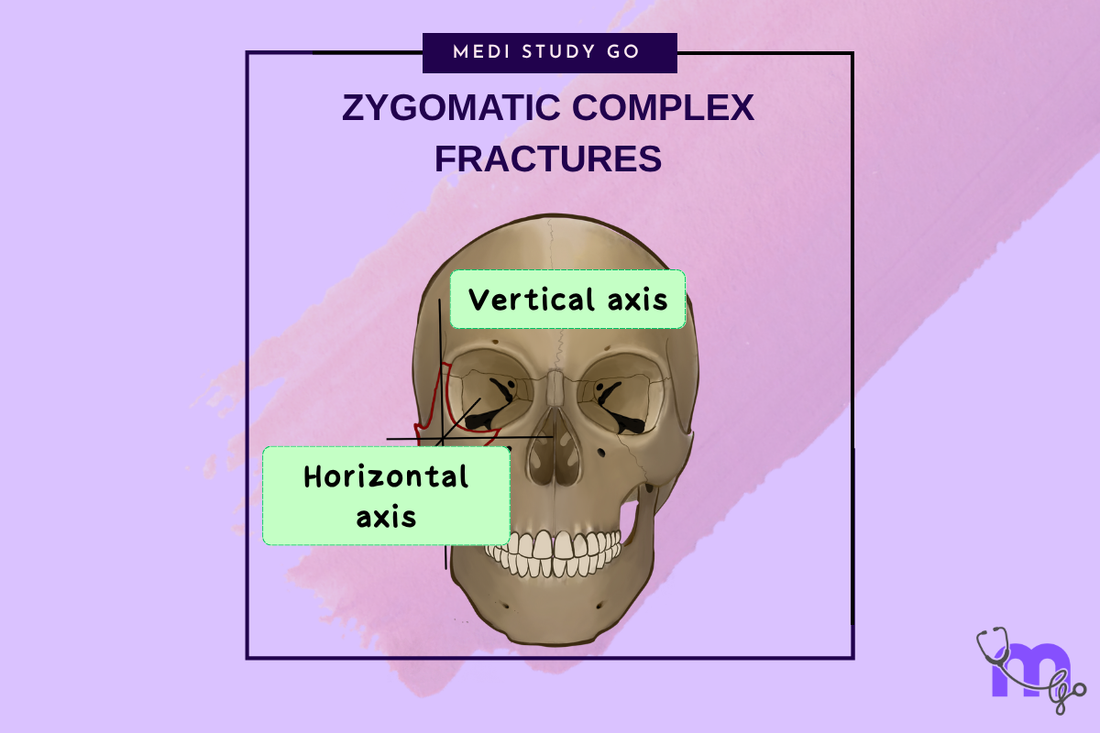
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Gillies Temporal Approach in Zygomatic Arch Fractures
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Mandibular Fractures: Classification Systems and Clinical Relevance
Champy's Lines of Osteosynthesis: Principles and Application
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Basic Principles of Fracture Fixation in Maxillofacial Surgery
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- Zygomatic complex fractures involve multiple anatomical structures requiring comprehensive assessment
- Knight and North classification guides treatment planning based on displacement patterns
- Three-point fixation provides optimal stability for most zygomatic complex fractures
- Ophthalmologic evaluation is essential due to high incidence of associated orbital injuries
- Early surgical intervention optimizes functional and aesthetic outcomes
Introduction
Zygomatic complex fractures represent one of the most common facial injuries encountered in maxillofacial surgery, accounting for approximately 25% of all facial fractures. These injuries, often referred to as tripod or tetrapod fractures, involve disruption of the zygomatic bone's articulations with surrounding facial structures, creating complex three-dimensional deformities that affect both function and aesthetics.
The zygoma serves as a crucial structural pillar of the midface, contributing to facial width, malar prominence, and orbital integrity. Its strategic position makes it vulnerable to trauma while simultaneously making fractures highly visible and functionally significant. The bone's multiple articulations with the frontal, temporal, maxillary, and sphenoid bones create predictable fracture patterns that require systematic evaluation and treatment.
Understanding zygomatic complex fractures requires comprehensive knowledge of three-dimensional anatomy, biomechanical principles, and surgical techniques. The complexity of these injuries often necessitates multi-point fixation and careful attention to restoration of facial contour and orbital function.
Anatomy and Fracture Patterns
Zygomatic Articulations
The zygoma articulates with four facial bones through distinct suture lines that represent areas of weakness during trauma. The frontozygomatic suture connects to the frontal bone, the zygomaticomaxillary suture joins the maxilla, the zygomaticotemporal suture articulates with the temporal bone, and the zygomaticosphenoid suture connects to the greater wing of the sphenoid.
These articulations create the classic "tripod" or "tetrapod" fracture pattern when disrupted simultaneously. The infraorbital rim involvement adds complexity by potentially affecting orbital volume and extraocular muscle function.
Classification Systems

The Knight and North classification system categorizes zygomatic complex fractures into six groups based on displacement and rotational patterns. Group I involves no significant displacement, Group II includes isolated arch fractures, Groups III-V describe various rotational patterns, and Group VI encompasses comminuted fractures with additional fracture lines.
This classification helps predict surgical complexity and guides treatment planning. Understanding rotational patterns is particularly important as they determine the reduction technique and fixation requirements.
Clinical Assessment and Diagnosis

Physical Examination
Clinical evaluation begins with systematic inspection for facial asymmetry, periorbital edema, and malar flattening. Palpation may reveal step defects at the infraorbital rim, frontozygomatic suture, and zygomatic arch. The presence of trismus suggests zygomatic arch impingement on the coronoid process.
Ophthalmologic assessment is crucial due to the high incidence of associated orbital injuries. Approximately 30% of zygomatic complex fractures involve significant orbital complications, including diplopia, enophthalmos, and globe injuries.
What are the pathognomonic signs of zygomatic complex fractures?
The classic triad of zygomatic complex fractures includes malar flattening, infraorbital nerve paresthesia, and diplopia. Malar flattening results from posterior and medial displacement of the zygomatic body, creating loss of cheek projection and facial asymmetry.
Infraorbital nerve paresthesia occurs due to nerve compression or injury at the infraorbital foramen, causing numbness in the distribution of the nerve. Diplopia may result from orbital floor involvement, extraocular muscle entrapment, or changes in orbital volume.
These findings, combined with radiographic confirmation, establish the diagnosis and guide treatment planning decisions.
Imaging Studies
CT imaging with multiplanar reconstructions provides detailed visualization of fracture patterns and displacement. Coronal images are particularly valuable for assessing orbital floor integrity and extraocular muscle position. Three-dimensional reconstructions facilitate surgical planning and patient education.
Key radiographic findings include discontinuity at zygomatic sutures, zygomatic arch depression, and orbital floor defects. The relationship between fracture segments and the degree of displacement guide treatment decisions.
Surgical Management

Treatment Principles
Treatment goals include restoration of facial width and projection, correction of orbital volume, reestablishment of zygomatic arch continuity, and preservation of extraocular muscle function. These objectives require accurate reduction and stable fixation of displaced fragments.
The timing of intervention typically falls within the first two weeks post-injury, allowing initial swelling to subside while preventing significant scarring. Earlier intervention may be necessary for severe displacement or functional deficits.
Surgical Approaches
Multiple surgical approaches may be necessary to access all fracture sites adequately. The transconjunctival approach provides excellent access to the orbital floor with minimal visible scarring. Upper and lower eyelid approaches offer good visualization but carry higher risks of complications.
Intraoral approaches through the maxillary vestibule allow access to the zygomaticomaxillary buttress and infraorbital rim. Coronal approaches may be necessary for complex fractures involving the zygomatic arch or temporal region.
Reduction Techniques
Reduction methods vary based on fracture pattern and displacement severity. The Gillies temporal approach uses a temporal incision and specialized elevators to reduce zygomatic arch fractures through a minimally invasive technique.
For complex zygomatic body fractures, direct visualization through multiple approaches may be necessary. Reduction typically involves disimpaction of telescoped fragments followed by restoration of anatomical relationships.
Fixation Methods
Miniplate Fixation
Contemporary fixation techniques favor rigid internal fixation with titanium miniplates and screws. The number and location of fixation points depend on fracture stability and displacement patterns. Most zygomatic complex fractures require fixation at the frontozygomatic suture and zygomaticomaxillary buttress.
Three-point fixation, including the infraorbital rim, provides optimal stability for most displaced fractures. The use of 1.5mm or 2.0mm miniplate systems offers adequate strength while minimizing bulk and palpability.
How many fixation points are required for stable zygomatic complex fractures?
Most zygomatic complex fractures require two to three points of fixation for optimal stability. The frontozygomatic suture and zygomaticomaxillary buttress represent the most critical fixation sites, providing resistance to rotational displacement.
Addition of infraorbital rim fixation creates three-point fixation, which is recommended for unstable fractures or those with significant comminution. The greater wing of the sphenoid provides the most reliable landmark for assessing adequate reduction.
Four-point fixation, including the zygomatic arch, may be necessary for severely comminuted fractures or those with persistent instability after three-point fixation.
Complications and Management
Early Complications
Early complications include persistent diplopia, enophthalmos, infraorbital nerve dysfunction, and hardware complications. Diplopia may result from inadequate orbital floor reconstruction or extraocular muscle entrapment requiring surgical exploration.
Enophthalmos typically results from inadequate restoration of orbital volume or posterior displacement of the zygomatic body. Prevention through accurate reduction and appropriate fixation is preferable to secondary correction.
Late Complications
Late complications include chronic pain, facial asymmetry, and functional deficits. Malunion may require secondary osteotomies and repositioning, which is technically challenging and may not achieve optimal results.
Hardware-related complications include plate exposure, infection, and palpability. These issues may require hardware removal after adequate healing has occurred.
Outcomes and Prognosis
Most patients achieve satisfactory functional and aesthetic outcomes following appropriate treatment of zygomatic complex fractures. Residual symptoms are common but typically mild, including minor asymmetry or numbness.
Long-term follow-up is important for detecting late complications and ensuring optimal healing. Patient satisfaction is generally high when realistic expectations are established and comprehensive treatment is provided.
Conclusion
Zygomatic complex fractures require comprehensive understanding of three-dimensional anatomy and careful attention to both functional and aesthetic outcomes. Modern treatment emphasizes accurate reduction and stable internal fixation to achieve optimal results.
The key to successful management lies in systematic evaluation, appropriate surgical planning, and meticulous technique. Understanding the relationship between anatomy, fracture patterns, and treatment approaches enables optimal patient care and successful outcomes in these challenging injuries.