Basic Principles of Fracture Fixation in Maxillofacial Surgery
Medi Study Go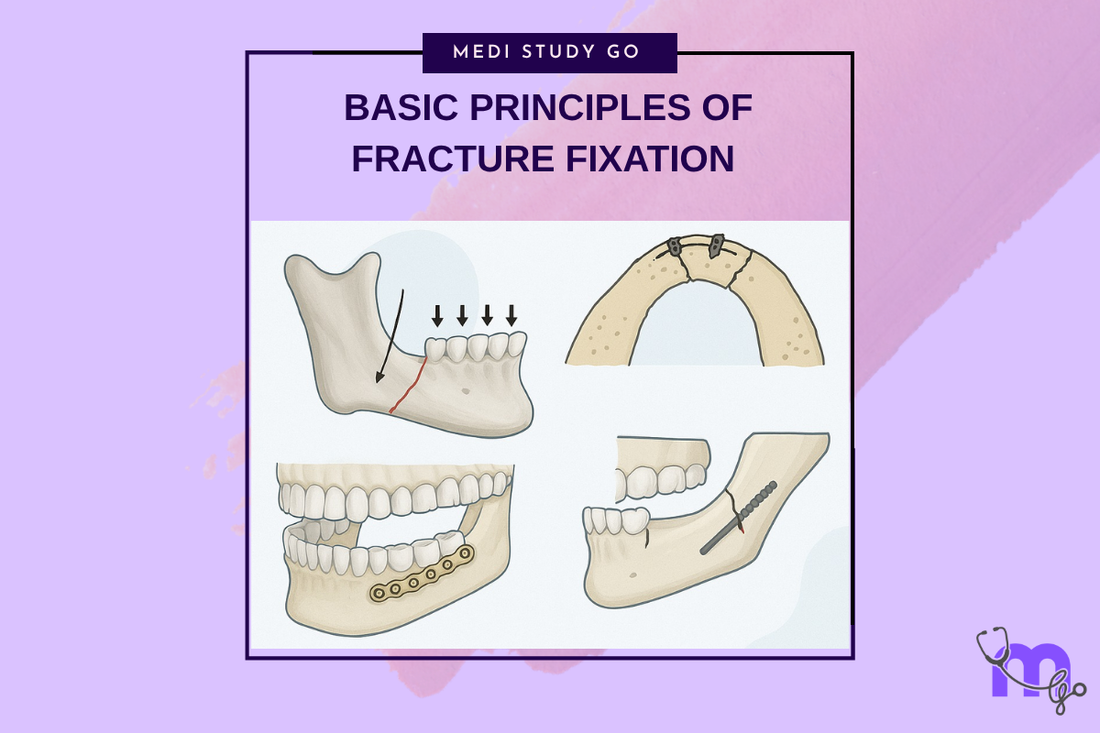
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Gillies Temporal Approach in Zygomatic Arch Fractures
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Mandibular Fractures: Classification Systems and Clinical Relevance
Champy's Lines of Osteosynthesis: Principles and Application
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- The fundamental principles of fracture fixation are reduction, fixation, immobilization, and early return of function
- Understanding force vectors and biomechanics is essential for successful fracture management
- Rigid internal fixation has revolutionized maxillofacial trauma treatment by enabling immediate function
- Load-sharing versus load-bearing concepts guide fixation method selection
- Proper application of AO principles optimizes healing and minimizes complications
Introduction
The management of maxillofacial fractures has evolved dramatically over the past century, transitioning from prolonged immobilization techniques to sophisticated internal fixation systems that promote early functional recovery. Understanding the fundamental principles underlying fracture fixation is essential for achieving optimal outcomes in maxillofacial trauma surgery.
The development of rigid internal fixation principles, largely based on AO (Arbeitsgemeinschaft für Osteosynthesefragen) concepts, has revolutionized fracture treatment by emphasizing anatomical reduction, stable fixation, and early mobilization. These principles, originally developed for long bone fractures, have been successfully adapted to the unique requirements of facial bone surgery.
Modern fracture fixation in maxillofacial surgery requires understanding of biomechanical principles, material properties, healing biology, and surgical techniques. The integration of these concepts enables surgeons to select appropriate fixation methods and achieve predictable results while minimizing complications.
Fundamental Principles of Fracture Treatment
The Four Pillars of Fracture Management
The fundamental principles of fracture treatment include reduction, fixation, immobilization, and early return of function. These principles, established by the AO Foundation, provide a systematic approach to fracture management that optimizes healing while minimizing complications.
Reduction involves restoring normal anatomical relationships between fracture fragments. This may be achieved through closed manipulation or open surgical techniques, depending on fracture characteristics and displacement patterns.
Fixation provides mechanical stability to maintain reduction during the healing process. Modern fixation methods range from simple wire techniques to sophisticated plate and screw systems designed for specific anatomical regions and loading conditions.
Immobilization prevents displacement of fracture fragments during healing while allowing controlled motion that promotes bone remodeling. The concept has evolved from rigid immobilization to controlled mobilization that optimizes healing biology.
Early return of function minimizes complications associated with prolonged immobilization while promoting optimal healing through physiological loading. This principle has become increasingly important in contemporary fracture management.
What distinguishes open reduction from closed reduction techniques?
Open reduction involves direct surgical exposure of fracture sites, allowing precise anatomical restoration under direct visualization. This approach enables accurate reduction of complex fractures and provides access for internal fixation placement.
Closed reduction achieves fracture alignment through indirect manipulation without surgical exposure. While less invasive, this approach may be limited in complex fractures and typically requires external immobilization methods.
The choice between approaches depends on fracture complexity, displacement, associated injuries, and functional requirements. Modern practice increasingly favors open reduction for displaced facial fractures due to superior outcomes.
Biomechanical Principles
Force Vectors and Stress Distribution
Understanding force transmission through facial bones is crucial for effective fixation design. The facial skeleton functions as an integrated framework where forces are distributed through predictable pathways during normal function.
Masticatory forces can exceed 200 pounds per square inch in the molar region, creating significant stress patterns throughout the facial skeleton. These forces must be considered when designing fixation systems to ensure adequate strength and durability.
Load-Sharing vs. Load-Bearing Concepts
Load-sharing fixation allows forces to be distributed between the healing bone and the fixation hardware. This concept, exemplified by Champy's miniplate technique, permits some micromotion that may promote bone healing while providing adequate stability.
Load-bearing fixation requires the hardware to carry the entire functional load until bone healing occurs. This approach, using larger reconstruction plates, is necessary for severely comminuted fractures or cases with significant bone loss.
The selection between approaches depends on fracture stability, bone quality, and expected loading conditions. Understanding these concepts guides appropriate fixation selection for specific clinical situations.
Fixation Methods and Materials
Wire Fixation Techniques
Wire fixation represents the historical foundation of maxillofacial fracture treatment and remains useful in specific circumstances. Transosseous wiring provides simple, effective fixation for stable fracture patterns while maintaining low cost and technical simplicity.
The technique requires understanding of wire properties, knotting techniques, and anatomical considerations to achieve optimal results. Proper wire placement and tension are crucial for maintaining reduction while avoiding tissue damage.
Miniplate Systems
Miniplate fixation has become the standard of care for most facial fractures due to its versatility, strength, and biocompatibility. These systems provide rigid fixation while minimizing hardware bulk and tissue trauma.
The development of various plate configurations, including straight plates, L-plates, and curved designs, allows adaptation to different anatomical sites and fracture patterns. Understanding plate selection and contouring principles is essential for optimal results.
Reconstruction Plates
Heavy reconstruction plates are reserved for cases requiring load-bearing fixation, such as severely comminuted fractures or mandibular continuity defects. These systems provide maximum strength but require careful surgical technique to avoid complications.
The use of reconstruction plates often necessitates external approaches and may require secondary procedures for optimal functional and aesthetic results. Understanding indications and limitations is crucial for appropriate application.
Surgical Techniques and Considerations
Anatomical Reduction Principles
Achieving anatomical reduction requires systematic approach to fracture alignment, beginning with restoration of facial height, width, and projection. This sequence ensures proper three-dimensional relationships and facilitates subsequent reductions.
Key reference points include the infraorbital rims, zygomatic arches, and dental occlusion. Restoration of these landmarks guides overall facial reconstruction and provides stable foundations for complex repairs.
Hardware Selection and Placement
Appropriate hardware selection depends on multiple factors including fracture location, bone quality, expected forces, and patient factors. Understanding the mechanical properties of different systems guides optimal selection for specific applications.
Plate positioning should follow established biomechanical principles while considering anatomical constraints and aesthetic factors. Proper screw placement and length selection are crucial for achieving adequate fixation strength.
How do monocortical and bicortical screw techniques differ?
Monocortical screws engage only the near cortex and are sufficient for most facial bone applications when plates are properly positioned. They minimize the risk of injury to deep structures while providing adequate holding power.
Bicortical screws engage both cortices and provide maximum holding strength but carry higher risks of nerve or vessel injury. They are typically reserved for reconstruction plates or cases with poor bone quality.
The choice depends on anatomical location, bone thickness, proximity to vital structures, and required holding strength. Understanding these factors guides appropriate screw selection for specific applications.
Biological Considerations
Bone Healing Mechanisms
Successful fracture fixation requires understanding of bone healing biology and factors that influence the healing process. Primary bone healing occurs with rigid fixation and perfect reduction, while secondary healing involves callus formation.
The rich vascular supply of facial bones generally promotes rapid healing, with most fractures achieving clinical union within 4-6 weeks. However, factors such as infection, poor reduction, and patient factors can significantly affect healing outcomes.
Factors Affecting Healing
Multiple factors influence bone healing including patient age, nutrition, smoking status, medical comorbidities, and medication use. Understanding these factors helps predict healing potential and guides treatment selection.
Local factors such as infection, soft tissue damage, and hardware-related issues can also affect healing outcomes. Optimization of these factors through proper surgical technique and postoperative care is essential for success.
Complications and Prevention
Hardware-Related Complications
Common hardware complications include infection, loosening, fracture, and exposure. Understanding risk factors and prevention strategies minimizes complication rates and optimizes patient outcomes.
Proper surgical technique, appropriate hardware selection, and careful patient selection are key factors in preventing hardware complications. When complications occur, prompt recognition and treatment are essential for optimal management.
Technical Errors and Prevention
Technical errors in fixation can lead to poor outcomes and complications. Common errors include inadequate reduction, improper hardware selection, poor plate contouring, and incorrect screw placement.
Prevention requires thorough understanding of anatomical relationships, biomechanical principles, and surgical techniques. Careful preoperative planning and attention to technical details minimize error rates.
Contemporary Developments
Advanced Materials and Technology
Modern developments in fixation technology include biodegradable plates, patient-specific implants, and advanced titanium alloys. These innovations aim to improve biocompatibility while maintaining mechanical properties.
Computer-assisted surgical planning and navigation systems enhance precision in hardware placement and may improve outcomes in complex cases. Understanding these technologies and their applications is increasingly important for contemporary practice.
Minimally Invasive Techniques
The trend toward minimally invasive surgery has influenced fracture fixation techniques, with emphasis on smaller incisions, endoscopic approaches, and percutaneous fixation methods where appropriate.
These techniques aim to minimize surgical trauma while maintaining fixation quality. However, they require specialized training and may not be appropriate for all fracture patterns or patient populations.
Future Directions
Biological Enhancement
Future developments may focus on biological enhancement of fracture healing through growth factors, stem cell therapy, and tissue engineering approaches. These technologies may accelerate healing and improve outcomes in challenging cases.
The integration of biological and mechanical approaches represents an exciting area for future development in fracture fixation technology and technique refinement.
Smart Implants and Monitoring
Emerging technologies include smart implants with sensing capabilities and remote monitoring systems that could provide real-time information about healing progress and hardware performance.
These developments may enable personalized treatment approaches and early detection of complications, potentially improving outcomes while reducing the need for routine follow-up procedures.
Conclusion
The principles of fracture fixation in maxillofacial surgery continue to evolve with advancing understanding of biomechanics, materials science, and healing biology. However, the fundamental concepts of anatomical reduction, stable fixation, and early function remain central to successful treatment.
Understanding these principles and their appropriate application enables surgeons to achieve optimal outcomes while minimizing complications. The integration of traditional techniques with modern technology and materials provides unprecedented opportunities for improving patient care.
Future developments will likely focus on biological enhancement, minimally invasive techniques, and smart technologies that further optimize fracture healing and functional outcomes. However, mastery of fundamental principles will remain essential for successful clinical practice.