Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Medi Study Go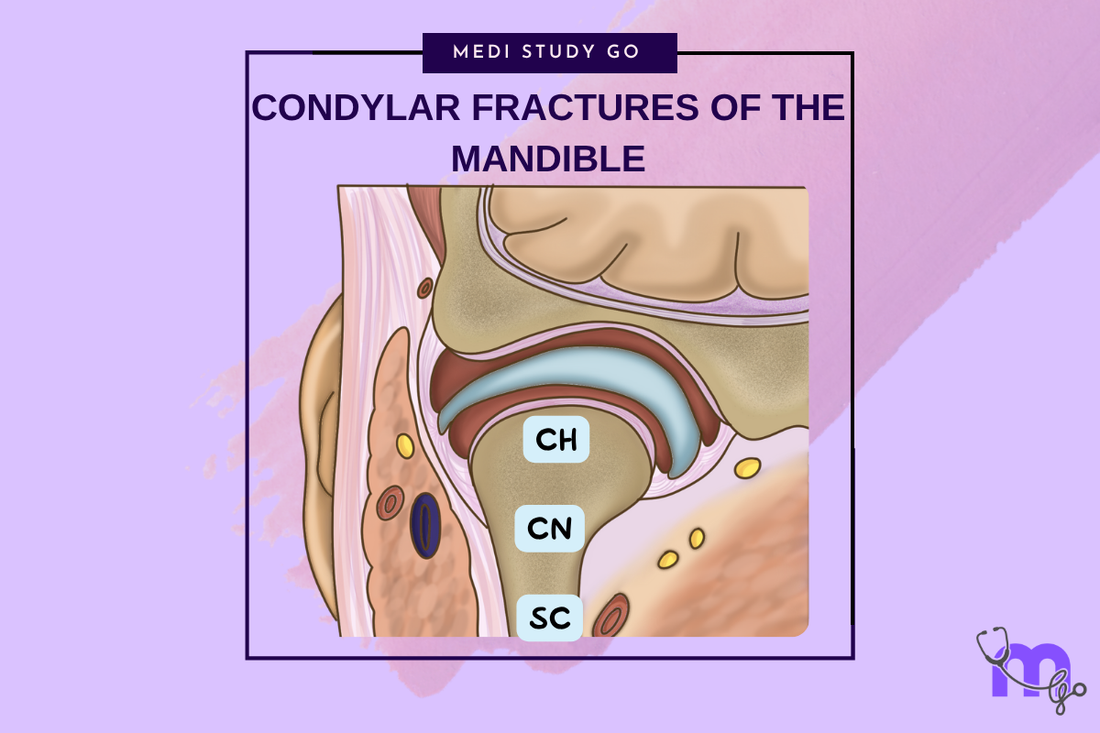
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Gillies Temporal Approach in Zygomatic Arch Fractures
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Mandibular Fractures: Classification Systems and Clinical Relevance
Champy's Lines of Osteosynthesis: Principles and Application
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Basic Principles of Fracture Fixation in Maxillofacial Surgery
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- Condylar fractures account for 25-35% of all mandibular fractures with unique treatment considerations
- Classification systems guide treatment decisions between conservative and surgical management
- Absolute surgical indications include displacement into middle cranial fossa and foreign body presence
- Conservative treatment with functional therapy achieves excellent outcomes in most cases
- Age significantly influences treatment approach and healing potential
Introduction
Condylar fractures of the mandible represent a unique subset of maxillofacial trauma characterized by complex anatomy, controversial treatment approaches, and significant functional implications. These injuries account for 25-35% of all mandibular fractures and present distinctive challenges due to the critical role of the temporomandibular joint in mandibular function.
The management of condylar fractures remains one of the most debated topics in maxillofacial surgery, with ongoing controversy regarding surgical versus conservative treatment approaches. The decision-making process requires careful consideration of multiple factors including patient age, fracture pattern, displacement, associated injuries, and functional requirements.
Understanding condylar fractures requires comprehensive knowledge of temporomandibular joint anatomy, biomechanics, and healing biology. The unique characteristics of this region create specific challenges for both diagnosis and treatment that distinguish condylar fractures from other mandibular injuries.
Anatomy and Classification

Temporomandibular Joint Anatomy
The temporomandibular joint consists of the mandibular condyle, glenoid fossa, articular disc, and associated ligaments and muscles. The condylar head articulates with the glenoid fossa through the interposed articular disc, creating a complex joint that allows both rotational and translational movements.
The condylar neck represents the constricted area below the condylar head where most fractures occur. This region's relatively narrow cross-sectional area and position make it vulnerable to fracture forces while serving as a crucial component of mandibular biomechanics.
MacLennan Classification
The MacLennan classification system categorizes condylar fractures based on fracture fragment relationships: no displacement, deviation, displacement, and dislocation. This system provides a framework for treatment decision-making and outcome prediction.
No displacement fractures maintain normal anatomical relationships, while deviation involves angulation without loss of contact. Displacement creates overlap or gap between fragments, and dislocation involves complete separation with condylar head displacement from the glenoid fossa.
What factors determine the level of condylar fractures?
The level of condylar fractures is determined by the point of force application and energy transmission patterns. Intracapsular fractures occur within the joint capsule and typically involve the condylar head. Extracapsular fractures occur below the capsule and may be further classified as high or low subcondylar fractures.
High subcondylar fractures occur at the condylar neck level, while low subcondylar fractures involve the region between the neck and mandibular angle. The fracture level influences treatment approaches and surgical accessibility.
Clinical Presentation and Diagnosis

Signs and Symptoms
Patients with condylar fractures present with characteristic findings including preauricular pain, swelling, limited mouth opening, and deviation of the mandible toward the fractured side during opening. Malocclusion is common, particularly in bilateral cases.
The classic triad includes limitation of mandibular movement, deviation during opening, and malocclusion. However, the severity of symptoms varies considerably depending on fracture pattern, displacement, and associated injuries.
Diagnostic Imaging
Panoramic radiography provides initial screening for condylar fractures but may miss minimally displaced or intracapsular fractures. CT scanning with multiplanar reconstructions offers superior visualization of fracture patterns and displacement.
MRI may provide valuable information about disc position and soft tissue injuries but is not routinely necessary for treatment planning. The relationship between imaging findings and clinical symptoms guides treatment decisions.
Functional Assessment
Evaluation of mandibular function includes assessment of mouth opening, lateral excursions, and protrusive movements. The pattern of limitation helps determine the extent of functional impairment and guides treatment selection.
Joint sounds, including clicking or crepitus, may indicate disc displacement or joint surface irregularities. However, these findings must be interpreted in the context of overall clinical presentation and imaging studies.
Treatment Decision Making
Conservative vs. Surgical Management
The decision between conservative and surgical treatment remains controversial and depends on multiple factors including fracture pattern, displacement, patient age, functional requirements, and surgeon experience.
Conservative treatment involves a period of rest followed by progressive functional therapy to restore mandibular movement. This approach relies on the joint's adaptive capacity and the body's natural healing mechanisms.
Absolute Surgical Indications
Certain conditions mandate surgical intervention regardless of other factors. These absolute indications include displacement of the condylar head into the middle cranial fossa, presence of foreign bodies in the joint space, and impossibility of obtaining adequate occlusion by closed means.
Lateral extracapsular displacement of the condylar head also requires surgical reduction due to the inability to achieve adequate healing in this position through conservative means.
Relative Surgical Indications
Relative indications for surgery include bilateral condylar fractures in edentulous patients, unilateral fractures with severe displacement, and cases where adequate function cannot be achieved through conservative treatment.
The decision in these cases requires careful weighing of potential benefits against surgical risks and consideration of individual patient factors and expectations.
Conservative Treatment Approaches

Functional Therapy Protocol
Conservative treatment typically involves a brief period of rest (7-10 days) followed by progressive functional therapy. The protocol emphasizes early mobilization to prevent ankylosis while allowing adequate healing time.
Physical therapy includes range-of-motion exercises, muscle strengthening, and dietary modifications. The program is gradually advanced based on patient comfort and healing progress.
Outcomes of Conservative Treatment
Studies consistently demonstrate excellent outcomes with conservative treatment for most condylar fractures. Patient satisfaction rates exceed 90% in most series, with good restoration of mandibular function and minimal long-term complications.
The adaptive capacity of the temporomandibular joint allows functional compensation even in cases with significant anatomical disruption. Long-term studies show stable results with conservative management.
Surgical Treatment Approaches
Surgical Access Routes
Multiple surgical approaches are available for condylar fracture repair, each with specific advantages and limitations. The preauricular approach provides direct access to the joint but carries risks of facial nerve injury and auricular complications.
The endaural approach offers good access through the external auditory canal, while the submandibular approach allows access to subcondylar fractures with lower nerve injury risk but limited visualization of high fractures.
What are the primary risks of surgical treatment for condylar fractures?
The primary risks of surgical treatment include facial nerve injury (particularly the temporal and marginal mandibular branches), hearing loss, scarring, infection, and hardware complications. The risk of permanent facial nerve weakness ranges from 2-15% depending on the approach used.
Additional risks include inadequate reduction, hardware failure, and temporomandibular joint dysfunction. These complications must be weighed against potential benefits when considering surgical intervention.
Fixation Methods
Various fixation methods are available including miniplates, lag screws, and specialized condylar fixation systems. The choice depends on fracture pattern, bone quality, and surgeon preference.
Two-point fixation is generally preferred for optimal stability, though single-point fixation may be adequate for stable fracture patterns. The fixation must be positioned to avoid interference with joint function.
Pediatric Considerations
Growth and Development
Condylar fractures in children present unique challenges due to ongoing growth and development. The condylar growth center is crucial for mandibular development, and injury may result in growth disturbances.
Conservative treatment is generally preferred in pediatric patients to minimize growth interference. However, severe displacement or functional impairment may require surgical intervention despite growth considerations.
Long-term Outcomes in Children
Long-term studies of pediatric condylar fractures show generally favorable outcomes with conservative treatment. Most children adapt well to anatomical changes and maintain good mandibular function.
Growth disturbances may occur but are often minimal and well-compensated. Regular long-term follow-up is important to monitor growth and development patterns.
Complications and Long-term Outcomes
Early Complications
Early complications of condylar fractures include infection, nerve injury, inadequate reduction, and hardware complications in surgically treated cases. Conservative treatment has lower early complication rates but may result in initial functional limitations.
Ankylosis represents a serious complication that may occur with either treatment approach but is more common with prolonged immobilization or inadequate mobilization.
Late Complications
Long-term complications include temporomandibular joint dysfunction, chronic pain, limited mouth opening, and facial asymmetry. These complications may occur regardless of treatment method but are generally more common with severe initial displacement.
Degenerative joint disease may develop over time, particularly in cases with significant anatomical disruption. However, most patients remain asymptomatic despite radiographic changes.
Factors Affecting Outcomes
Several factors influence treatment outcomes including patient age, fracture pattern, displacement severity, associated injuries, and treatment compliance. Younger patients generally have better adaptive capacity and outcomes.
The presence of bilateral fractures, edentulous state, and medical comorbidities may negatively affect outcomes and influence treatment selection.
Future Directions
Technological Advances
Advances in imaging technology, surgical techniques, and implant design continue to improve treatment options for condylar fractures. Three-dimensional planning and patient-specific implants may enhance surgical outcomes.
Minimally invasive surgical techniques and improved fixation systems may reduce complications while maintaining treatment effectiveness. Endoscopic approaches show promise for selected cases.
Research Priorities
Ongoing research focuses on optimal treatment selection criteria, long-term outcome predictors, and development of improved treatment protocols. Comparative studies between treatment approaches continue to provide evidence for decision-making.
The role of biological factors in healing and adaptation requires further investigation to optimize treatment approaches and outcomes.
Conclusion
Condylar fractures of the mandible represent complex injuries requiring individualized treatment approaches based on multiple factors. The controversy regarding optimal treatment continues to drive research and clinical innovation in this field.
Conservative treatment remains the standard of care for most condylar fractures, with excellent long-term outcomes in appropriately selected cases. Surgical intervention should be reserved for specific indications where conservative treatment is unlikely to succeed.
The key to successful management lies in careful patient evaluation, appropriate treatment selection, and comprehensive follow-up care. Understanding the natural history and adaptive capacity of the temporomandibular joint guides treatment decisions and outcome expectations.