Champy’s Lines of Osteosynthesis: Principles and Application
Medi Study Go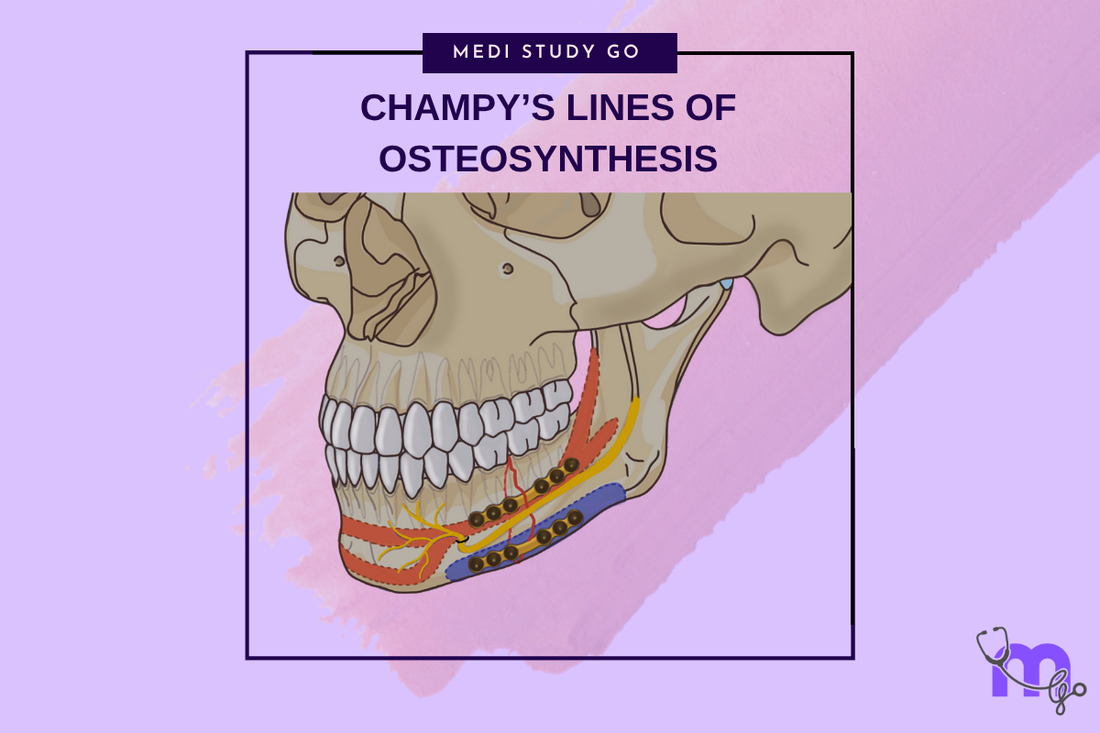
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Gillies Temporal Approach in Zygomatic Arch Fractures
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Mandibular Fractures: Classification Systems and Clinical Relevance
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Basic Principles of Fracture Fixation in Maxillofacial Surgery
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- Champy's lines represent optimal locations for mandibular fracture fixation based on biomechanical principles
- The concept of ideal osteosynthesis lines minimizes hardware requirements while maximizing stability
- Understanding tension and compression zones is crucial for proper plate placement
- Single miniplate fixation along Champy's lines provides adequate stability for most mandibular fractures
- Proper application requires knowledge of mandibular biomechanics and anatomical landmarks
Introduction
The concept of ideal osteosynthesis lines, developed by Michel Champy and colleagues in the 1970s, revolutionized the treatment of mandibular fractures by introducing biomechanically based fixation principles. This groundbreaking work established scientific foundations for miniplate fixation and demonstrated that understanding mandibular biomechanics could optimize treatment while minimizing hardware requirements.
Champy's research identified specific lines along the mandible where single miniplate fixation provides optimal fracture stability. These "ideal osteosynthesis lines" correspond to areas of maximum tensile stress during mandibular function, where properly placed plates can neutralize deforming forces and maintain fracture reduction.
The clinical impact of Champy's work extends beyond technical innovation to fundamental changes in treatment philosophy. By demonstrating that single miniplate fixation could achieve results comparable to more extensive hardware, Champy's principles enabled less invasive surgery with reduced morbidity and faster recovery times.
Biomechanical Foundations
Mandibular Stress Patterns
The mandible functions as a complex lever system subjected to multiple force vectors during mastication and function. These forces create predictable stress patterns with areas of tension, compression, and neutral zones that vary depending on the loading conditions and anatomical region.
During normal function, the superior border of the mandible experiences tensile forces while the inferior border undergoes compression. This stress distribution creates a neutral zone between tension and compression areas where forces are minimized. Understanding these patterns is essential for optimal fixation placement.
Tension Band Principle
Champy's approach applies the tension band principle to mandibular fracture fixation. By placing miniplates along lines of maximum tension, the hardware acts as a tension band that converts tensile forces into compressive forces at the fracture site, promoting healing and maintaining stability.
This principle explains why single miniplate fixation can be effective when properly positioned. The plate neutralizes the primary deforming forces while allowing physiological compression at the fracture site during function.
Ideal Osteosynthesis Lines
What defines the superior Champy line in mandibular body fractures?
The superior Champy line for mandibular body fractures runs along the external oblique ridge at the level of the tooth roots, approximately 5mm below the alveolar crest. This line corresponds to the area of maximum tensile stress during mandibular function.
Proper placement along this line requires careful attention to root positions and anatomical landmarks. The plate should be positioned to avoid root damage while maintaining optimal biomechanical advantage for fracture stabilization.
Angle Region Fixation
In the mandibular angle region, the ideal osteosynthesis line follows the external oblique ridge, positioned as high as possible while avoiding the roots of the third molar. This placement provides optimal resistance to the rotational forces that commonly affect angle fractures.
The high placement also minimizes the risk of hardware complications and provides better access for plate removal if necessary. The biomechanical advantage of this position makes single miniplate fixation effective for most angle fractures.
Symphysis and Parasymphysis
The anterior mandible presents unique challenges due to the complex force patterns in this region. Champy's principles identify two lines for symphyseal fixation: a superior line at the level of the tooth roots and an inferior line near the inferior border.
The torsional forces in the anterior region often require two-point fixation to achieve adequate stability. The separation between plates should be at least 5mm to prevent stress concentration and hardware failure.
Clinical Application
Preoperative Planning
Successful application of Champy's principles requires careful preoperative planning based on fracture location, pattern, and individual anatomical considerations. The surgeon must identify the appropriate osteosynthesis line and plan the surgical approach accordingly.
Imaging studies help identify optimal plate placement locations and potential anatomical obstacles such as tooth roots or the inferior alveolar nerve. Three-dimensional planning may be beneficial for complex fractures or anatomical variations.
Surgical Technique
Proper surgical technique is essential for successful implementation of Champy's principles. The approach must provide adequate visualization of the osteosynthesis line while minimizing soft tissue trauma and preserving neurovascular structures.
Plate contouring should follow the natural mandibular anatomy without creating gaps or excessive tension. The use of monocortical screws is typically sufficient when plates are properly positioned along Champy's lines.
Plate Selection and Positioning
The selection of appropriate miniplate systems depends on fracture characteristics and individual patient factors. Standard 2.0mm miniplates are suitable for most applications, while larger plates may be necessary for comminuted or unstable fractures.
Plate positioning must be precise to achieve optimal biomechanical advantage. Small variations in placement can significantly affect fixation stability and treatment outcomes.
Modifications and Adaptations
Load-Sharing vs. Load-Bearing
Champy's original concept emphasized load-sharing fixation where the plate shares loads with the healing bone rather than carrying the entire functional load. This approach contrasts with load-bearing fixation where rigid plates carry all functional forces.
Load-sharing fixation allows some micromotion that may promote bone healing while providing adequate stability for fracture maintenance. This concept has influenced contemporary approaches to fracture fixation throughout the skeleton.
Contemporary Modifications
Modern adaptations of Champy's principles include the use of locking plate technology and patient-specific plate designs. These modifications maintain the biomechanical principles while adapting to evolving technology and individual patient requirements.
The development of absorbable plate systems has also been influenced by Champy's work, with manufacturers designing products specifically for placement along ideal osteosynthesis lines.
Advantages and Limitations
Benefits of Champy's Approach
The primary advantages of Champy's approach include reduced hardware requirements, minimized surgical trauma, faster recovery times, and excellent functional outcomes. Single miniplate fixation is technically simpler and more cost-effective than multi-point fixation systems.
The biomechanical foundation of the approach provides predictable results with low complication rates when properly applied. The reduced hardware bulk also minimizes patient discomfort and long-term complications.
How do Champy's principles compare to rigid fixation methods?
Champy's principles generally provide comparable stability to rigid fixation methods while using less hardware and creating less surgical trauma. The load-sharing concept may actually promote better bone healing than completely rigid fixation.
However, some fracture patterns may require more extensive fixation than Champy's principles provide. Severely comminuted fractures, pathological fractures, or cases with significant bone loss may need additional fixation points or different approaches.
Clinical Outcomes and Evidence
Research Validation
Extensive research has validated the effectiveness of Champy's principles for mandibular fracture treatment. Studies consistently demonstrate excellent outcomes with low complication rates when the principles are properly applied.
Long-term follow-up studies show stable results with minimal hardware-related complications. The approach has been adopted worldwide and forms the basis for contemporary mandibular fracture treatment protocols.
Complication Rates
Complication rates with Champy's approach are generally low, with most studies reporting infection rates below 5% and hardware failure rates below 2%. The minimally invasive nature of single miniplate fixation contributes to these favorable outcomes.
When complications occur, they are typically manageable and do not significantly affect long-term outcomes. The reduced hardware bulk makes plate removal straightforward when necessary.
Future Developments
Technology Integration
Modern developments in plate design, surgical planning, and fixation technology continue to build upon Champy's biomechanical principles. Computer-assisted planning and patient-specific implants represent natural extensions of the personalized approach implicit in Champy's work.
Three-dimensional planning systems now allow precise identification of optimal osteosynthesis lines based on individual anatomy and biomechanical modeling. These tools may further improve outcomes and reduce complications.
Research Directions
Ongoing research continues to refine understanding of mandibular biomechanics and optimal fixation strategies. Studies of bone healing, stress distribution, and long-term outcomes contribute to continuing evolution of treatment approaches.
The integration of biological factors with mechanical principles represents an important area for future development, potentially leading to even more effective and less invasive treatment approaches.
Conclusion
Champy's lines of osteosynthesis represent a fundamental advancement in mandibular fracture treatment, providing biomechanically sound principles that optimize outcomes while minimizing intervention. Understanding and proper application of these principles remain essential skills for maxillofacial surgeons.
The enduring influence of Champy's work demonstrates the value of scientific inquiry in advancing surgical practice. The biomechanical foundation provides a rational basis for treatment decisions and continues to guide development of new technologies and techniques.
Future evolution of mandibular fracture treatment will likely build upon Champy's principles while incorporating new technologies and deeper understanding of bone healing biology. The fundamental concepts of biomechanically based fixation will remain relevant regardless of technological advances.