Mandibular Fractures: Classification Systems and Clinical Relevance
Medi Study Go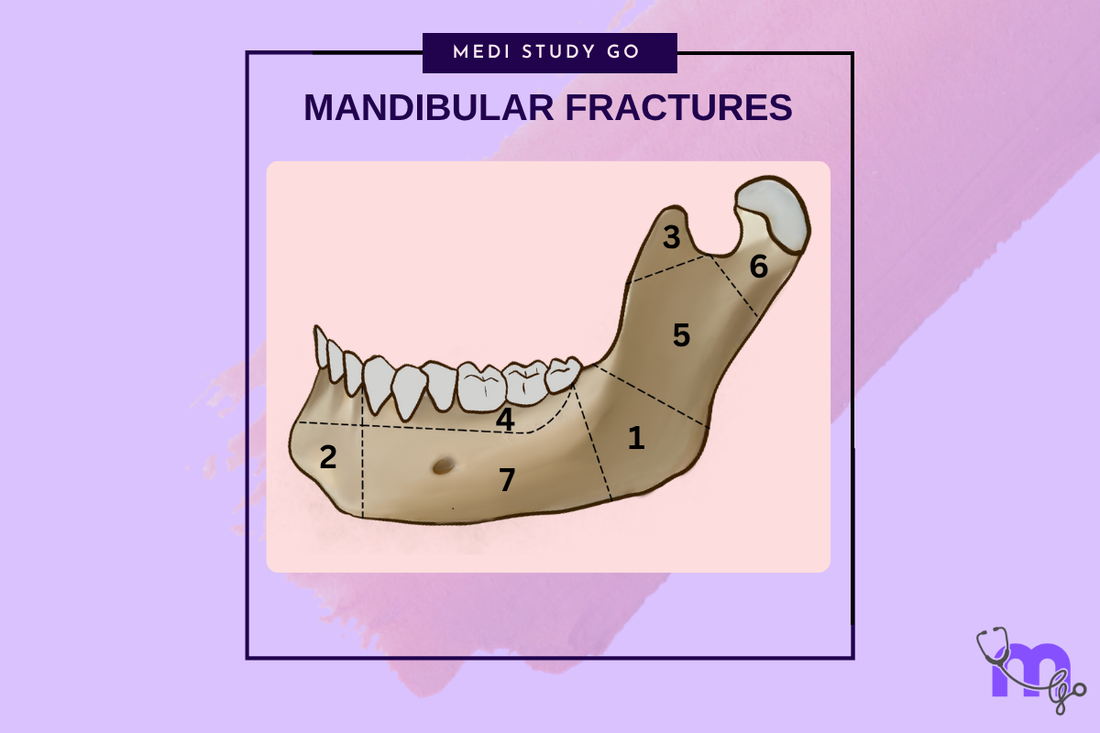
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Gillies Temporal Approach in Zygomatic Arch Fractures
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Champy's Lines of Osteosynthesis: Principles and Application
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Basic Principles of Fracture Fixation in Maxillofacial Surgery
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- Mandibular fractures are classified by anatomical location, morphology, and relationship to teeth
- The concept of favorable versus unfavorable fractures guides treatment decisions and prognosis
- Understanding muscle force vectors is crucial for predicting fracture displacement patterns
- Multiple classification systems exist, each serving different clinical and research purposes
- Proper classification facilitates treatment planning and outcome prediction
Introduction
Mandibular fractures represent the most common facial bone fractures, accounting for approximately 70% of all maxillofacial injuries. The mandible's prominent position and unique biomechanical properties make it vulnerable to trauma while simultaneously creating complex treatment challenges. Understanding the various classification systems for mandibular fractures is essential for effective communication, treatment planning, and outcome prediction.
The development of mandibular fracture classification systems reflects the evolution of maxillofacial surgery from empirical treatment to evidence-based practice. Early classifications focused primarily on anatomical location, while modern systems incorporate biomechanical principles, treatment implications, and prognostic factors.
Contemporary practice requires familiarity with multiple classification systems, each designed for specific purposes. Anatomical classifications guide surgical approaches, morphological systems predict treatment complexity, and functional classifications influence fixation strategies. The integration of these various systems provides comprehensive understanding necessary for optimal patient care.
Anatomical Classification Systems
Dingman and Natvig Classification
The Dingman and Natvig classification system divides the mandible into anatomical regions based on structural and functional considerations. This system identifies seven distinct regions: symphysis, parasymphysis, body, angle, ramus, coronoid process, and condylar process.
Each region has unique anatomical characteristics that influence fracture patterns, treatment approaches, and healing outcomes. The symphysis and parasymphysis regions involve the anterior mandible where muscle forces create complex displacement patterns. The body region extends from the mental foramen to the anterior border of the masseter muscle.
Regional Characteristics
The angle region, extending from the anterior border of the masseter to the posterior border of the mandible, represents the most common fracture site. This area's relative weakness, especially when third molars are present, creates a predisposition to fracture.
The ramus, coronoid, and condylar regions each present unique treatment challenges due to their anatomical relationships and functional importance. Understanding these regional characteristics guides treatment decision-making and approach selection.
Morphological Classifications

Kruger's General Classification
Kruger's classification system categorizes mandibular fractures based on morphological characteristics rather than anatomical location. This system includes simple (linear), greenstick, compound, comminuted, and pathological fractures.
Simple fractures involve clean breaks without significant tissue loss or contamination. Greenstick fractures occur primarily in children and involve incomplete bone fracture with cortical bending. Compound fractures communicate with the external environment, increasing infection risk and treatment complexity.
How do compound fractures differ from simple fractures in treatment requirements?
Compound fractures require more aggressive antibiotic therapy, careful wound debridement, and often immediate surgical intervention to prevent infection. The communication with the oral cavity or external environment creates bacterial contamination that simple fractures lack.
Treatment planning for compound fractures must consider soft tissue management, potential for infection, and the need for immediate stabilization to prevent further contamination. The complexity of these injuries often requires multidisciplinary management and extended antibiotic coverage.
Biomechanical Classifications
Favorable vs. Unfavorable Fractures
The concept of favorable versus unfavorable fractures represents one of the most clinically relevant classification concepts. This system considers the relationship between fracture line orientation and muscle force vectors to predict fracture stability and displacement patterns.
Favorable fractures have fracture lines oriented to resist displacement by muscle forces. The fracture geometry and muscle pull direction work together to maintain fracture reduction. Unfavorable fractures have orientations that promote displacement despite reduction efforts.
Muscle Force Considerations

Understanding muscle forces acting on the mandible is crucial for predicting fracture behavior. The masseter, temporalis, and medial pterygoid muscles create elevating forces, while the lateral pterygoid muscle produces protrusive forces. The suprahyoid muscles create depressing forces on the mandibular body.
These force vectors interact with fracture line orientation to determine fracture stability. Horizontal fractures in the body region are typically unfavorable because muscle forces tend to cause displacement, while vertical fractures may be favorable if properly reduced.
Functional Classifications
Occlusal Relationship Classifications
Fractures are classified based on their relationship to dental occlusion and functional requirements. This system recognizes that fractures affecting dental function require different treatment approaches than those that do not.
Fractures involving the dentoalveolar region directly affect occlusion and require careful attention to dental relationships during treatment. Fractures of the ramus or condyle may affect occlusion indirectly through changes in mandibular position or function.
AO/ASIF Classification
The AO/ASIF classification system provides a comprehensive approach to mandibular fracture classification using alphanumeric codes. This system includes information about anatomical location, morphology, and associated injuries.
The systematic approach facilitates research, outcome comparison, and treatment standardization. The classification includes modifiers for soft tissue involvement, displacement, and other factors relevant to treatment planning.
Clinical Applications
Treatment Planning Implications
Different classification systems provide different types of information relevant to treatment planning. Anatomical classifications guide surgical approach selection, while morphological classifications influence fixation strategies and healing expectations.
Understanding the clinical implications of each classification system enables surgeons to extract relevant information for treatment decision-making. The integration of multiple classification approaches provides comprehensive understanding necessary for optimal outcomes.
What factors determine the choice of fixation method in mandibular fractures?
The choice of fixation method depends on fracture location, morphology, displacement, patient factors, and surgeon preference. Anatomical location influences access and biomechanical requirements, while morphology affects stability and healing potential.
Favorable fractures may require only simple fixation techniques, while unfavorable fractures often need more robust fixation methods. Patient factors such as age, compliance, and medical status also influence fixation selection.
Contemporary Developments
Three-Dimensional Classifications
Modern imaging capabilities have enabled development of three-dimensional classification systems that better capture the complexity of mandibular fractures. These systems consider fracture patterns in multiple planes and provide more accurate assessment of injury severity.
Three-dimensional classifications may better predict treatment outcomes and guide reconstruction strategies in complex cases. The integration of imaging data with biomechanical analysis provides enhanced understanding of fracture behavior.
Outcome-Based Classifications
Recent developments focus on classifications that predict functional outcomes rather than simply describing anatomical features. These systems consider factors such as nerve involvement, soft tissue damage, and functional deficits.
Outcome-based classifications may prove more useful for treatment planning and patient counseling by providing realistic expectations for recovery and functional restoration.
Research and Documentation
Standardization Benefits
Standardized classification systems enable meaningful comparison of treatment outcomes across different institutions and patient populations. This standardization facilitates research, quality improvement, and evidence-based practice development.
The use of consistent terminology and classification criteria improves communication between clinicians and enhances the quality of scientific literature. Standardization also supports the development of treatment guidelines and protocols.
Database Development
Large-scale databases using standardized classification systems provide valuable insights into fracture patterns, treatment outcomes, and complication rates. These databases support evidence-based treatment recommendations and quality improvement initiatives.
The aggregation of classification data enables identification of trends, risk factors, and optimal treatment approaches for specific fracture patterns and patient populations.
Conclusion
Mandibular fracture classification systems serve multiple purposes in contemporary maxillofacial surgery practice. Understanding the various approaches and their clinical applications is essential for effective patient care, research participation, and professional communication.
The evolution of classification systems reflects advancing understanding of mandibular biomechanics, treatment principles, and outcome prediction. Future developments will likely integrate advanced imaging, biomechanical analysis, and outcome data to create more sophisticated and clinically relevant systems.
Successful application of classification systems requires understanding their strengths, limitations, and appropriate use in different clinical contexts. The integration of multiple classification approaches provides the comprehensive understanding necessary for optimal patient care and successful treatment outcomes.