Gillies Temporal Approach in Zygomatic Arch Fractures
Medi Study Go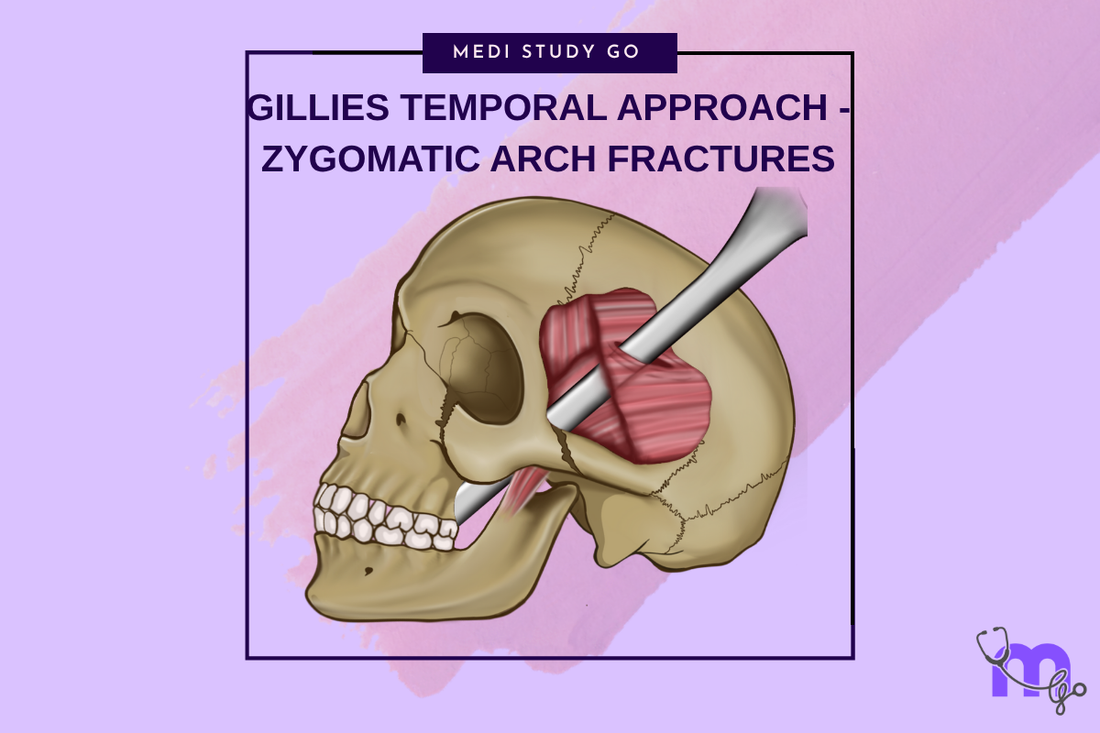
Related Resources
Comprehensive Guide to Maxillofacial Fractures in Oral Surgery
Le Fort Fractures: Classification, Clinical Features, and Management
Classification of Midfacial Fractures: Systems and Exam Tips
Zygomatic Complex Fractures: Diagnosis and Surgical Approaches
Orbital Blowout Fractures: Pathophysiology and Treatment Protocols
Mandibular Fractures: Classification Systems and Clinical Relevance
Champy's Lines of Osteosynthesis: Principles and Application
Mandibular Angle Fractures: Diagnosis, Complications, and Surgical Management
Condylar Fractures of the Mandible: Types, Indications for Surgery, and Outcomes
Basic Principles of Fracture Fixation in Maxillofacial Surgery
Dental Wiring Techniques in Maxillofacial Fracture Management
CSF Rhinorrhea in Maxillofacial Trauma: Causes, Diagnosis, and Management
Epistaxis Associated with Facial Fractures: Emergency Management
Complications of Maxillofacial Fractures: Early and Late Sequelae
Key Takeaways
- Gillies temporal approach provides minimally invasive access to zygomatic arch fractures
- Proper anatomical landmarks and instrument placement prevent temporal fascia injury
- The technique requires understanding of fascial planes and neurovascular anatomy
- Successful reduction depends on correct elevator positioning and manipulation techniques
- Complications are rare but include temporal branch facial nerve injury and inadequate reduction
Introduction
The Gillies temporal approach, first described by Sir Harold Gillies in 1927, remains the gold standard technique for closed reduction of zygomatic arch fractures. This minimally invasive approach provides excellent access to depressed zygomatic arch fractures while avoiding the extensive dissection and potential complications associated with open reduction techniques.
The elegance of the Gillies approach lies in its simplicity and effectiveness. By utilizing the natural fascial planes of the temporal region, surgeons can achieve adequate reduction of most zygomatic arch fractures through a small, well-concealed incision. The technique has stood the test of time due to its reliability, minimal morbidity, and excellent aesthetic outcomes.
Understanding the anatomical basis of this approach is crucial for successful implementation. The temporal fascia consists of superficial and deep layers that must be navigated carefully to avoid injury to the temporal branch of the facial nerve and the superficial temporal vessels. Proper instrument placement and manipulation techniques ensure effective reduction while minimizing complications.
Anatomical Considerations
Temporal Fascia Anatomy
The temporal region contains multiple fascial layers that create distinct anatomical planes. The superficial temporal fascia (temporoparietal fascia) contains the temporal branch of the facial nerve and superficial temporal vessels. The deep temporal fascia covers the temporalis muscle and provides the working space for the Gillies approach.
Between these fascial layers lies a loose areolar tissue plane that allows for safe dissection and instrument placement. Understanding these relationships is essential for avoiding injury to the facial nerve branches and achieving successful fracture reduction.
Zygomatic Arch Anatomy
The zygomatic arch is formed by the union of the temporal process of the zygomatic bone and the zygomatic process of the temporal bone. This bony bridge provides attachment for the masseter muscle and contributes to facial width and contour.
Fractures typically occur at the suture line or in the body of the arch, creating characteristic "V" or "W" shaped deformities. The degree of displacement and comminution influences the complexity of reduction and the likelihood of successful closed treatment.
Indications and Contraindications
When is the Gillies approach most appropriate for zygomatic arch fractures?
The Gillies temporal approach is most appropriate for isolated zygomatic arch fractures with minimal comminution and adequate bone stock for manipulation. Ideal candidates include patients with recent injuries (within 2-3 weeks) and sufficient arch displacement to allow elevator placement.
The approach works best for simple arch fractures without significant telescoping or complex comminution. Patients with good bone quality and minimal soft tissue scarring are most likely to achieve successful reduction with this technique.
Contraindications include severely comminuted fractures, chronic injuries with established malunion, and cases where adequate reduction cannot be achieved through closed means. The presence of associated zygomatic complex fractures may require additional open approaches for complete treatment.
Patient Selection Criteria
Successful outcomes depend on appropriate patient selection. Factors favoring the Gillies approach include isolated arch fractures, minimal soft tissue injury, and patient compliance with post-operative restrictions. Young patients with good healing potential typically achieve better outcomes than elderly patients with compromised bone quality.
The timing of intervention influences success rates. Early treatment within the first two weeks post-injury generally yields better results than delayed treatment when soft tissue scarring and early bone healing may complicate reduction efforts.
Surgical Technique

Preoperative Planning
Preoperative planning includes careful review of imaging studies to assess fracture pattern, displacement, and associated injuries. CT scans with three-dimensional reconstructions help visualize the fracture anatomy and plan the reduction strategy.
Patient positioning is critical for optimal access and visualization. The patient is positioned supine with the head turned away from the operative side. The temporal region is prepared and draped to provide adequate exposure while maintaining sterility.
Incision and Approach
The incision is placed approximately 2-2.5 cm superior and posterior to the external auditory canal, following the natural skin lines of the temporal region. The incision should be angled approximately 45 degrees to the zygomatic arch to provide optimal access.
Dissection proceeds through the subcutaneous tissue to the superficial temporal fascia. Care must be taken to identify and protect the temporal branch of the facial nerve, which lies within the superficial fascial layer. The dissection continues through the deep temporal fascia to expose the temporalis muscle.
Instrument Placement and Reduction
Specialized elevators, such as the Rowe zygomatic elevator or modified Bristow elevator, are used for fracture reduction. The elevator is placed beneath the zygomatic arch, typically at the most depressed portion of the fracture.
The reduction technique involves gentle elevation and lateral displacement of the fractured arch segments. Care must be taken to avoid excessive force that could cause further comminution or damage to surrounding structures. The reduction is typically performed in an upward, forward, and outward direction.
Technical Considerations
Instrument Selection
The choice of elevator depends on surgeon preference and fracture characteristics. The Rowe zygomatic elevator provides good leverage and control, while the Bristow elevator offers a different angle of approach. Some surgeons prefer custom-made elevators designed for specific anatomical requirements.
The elevator should be positioned to provide maximum mechanical advantage while minimizing the risk of slippage or tissue damage. Proper positioning requires understanding of the three-dimensional anatomy and fracture pattern.
Reduction Technique
Successful reduction requires careful attention to the direction and magnitude of force applied. The goal is to restore the normal contour of the zygomatic arch while avoiding over-reduction or inadequate correction.
The reduction is typically performed with controlled, steady pressure rather than sudden, forceful movements. Multiple attempts may be necessary to achieve optimal positioning, particularly in cases with significant displacement or comminution.
What are the key steps for successful fracture reduction?
The key steps for successful fracture reduction include proper instrument placement beneath the most depressed portion of the arch, gentle but firm elevation in the correct vector, and verification of adequate reduction through palpation and clinical assessment.
The reduction should restore the normal arch contour and eliminate any restriction of mandibular movement. Successful reduction is confirmed by restoration of facial symmetry and resolution of trismus if present.
Complications and Management
Intraoperative Complications
Intraoperative complications are uncommon but may include temporal branch facial nerve injury, superficial temporal vessel damage, and inadequate reduction. Nerve injury typically results from inappropriate dissection or instrument placement within the superficial fascial layer.
Vascular injury may cause significant bleeding and hematoma formation. Careful attention to anatomical planes and gentle tissue handling minimize the risk of these complications.
Postoperative Complications
Postoperative complications include infection, hematoma, inadequate reduction, and loss of reduction. Infection is rare due to the excellent blood supply of the temporal region. Hematoma formation may occur but typically resolves without intervention.
Inadequate reduction may require revision surgery or conversion to an open approach. Loss of reduction can occur if the fracture is unstable or if the patient does not comply with activity restrictions.
Outcomes and Follow-up
Expected Results
Most patients achieve excellent functional and aesthetic outcomes following successful Gillies temporal approach reduction. The restoration of facial contour and resolution of functional deficits occur gradually over several weeks as swelling subsides.
Long-term outcomes are generally favorable, with low rates of complications and high patient satisfaction. The minimal scarring and preserved facial nerve function contribute to excellent cosmetic results.
Postoperative Care
Postoperative care includes activity restrictions, ice application, and antibiotic prophylaxis as indicated. Patients should avoid vigorous chewing and contact sports for several weeks to prevent loss of reduction.
Follow-up examinations assess healing progress, functional recovery, and the maintenance of fracture reduction. Imaging studies may be obtained to confirm stable reduction and healing progress.
Conclusion
The Gillies temporal approach remains an excellent technique for the management of zygomatic arch fractures. Its minimally invasive nature, reliable outcomes, and low complication rates make it the preferred method for appropriately selected cases.
Success with this technique requires thorough understanding of the anatomical relationships, careful patient selection, and meticulous surgical technique. When performed correctly, the Gillies approach provides excellent functional and aesthetic outcomes with minimal morbidity.
Continued refinement of surgical techniques and instrumentation will likely further improve outcomes, but the fundamental principles established by Gillies nearly a century ago remain valid and effective for contemporary practice.