Cellular Adaptation: Types, Mechanisms, and Clinical Relevance
Medi Study Go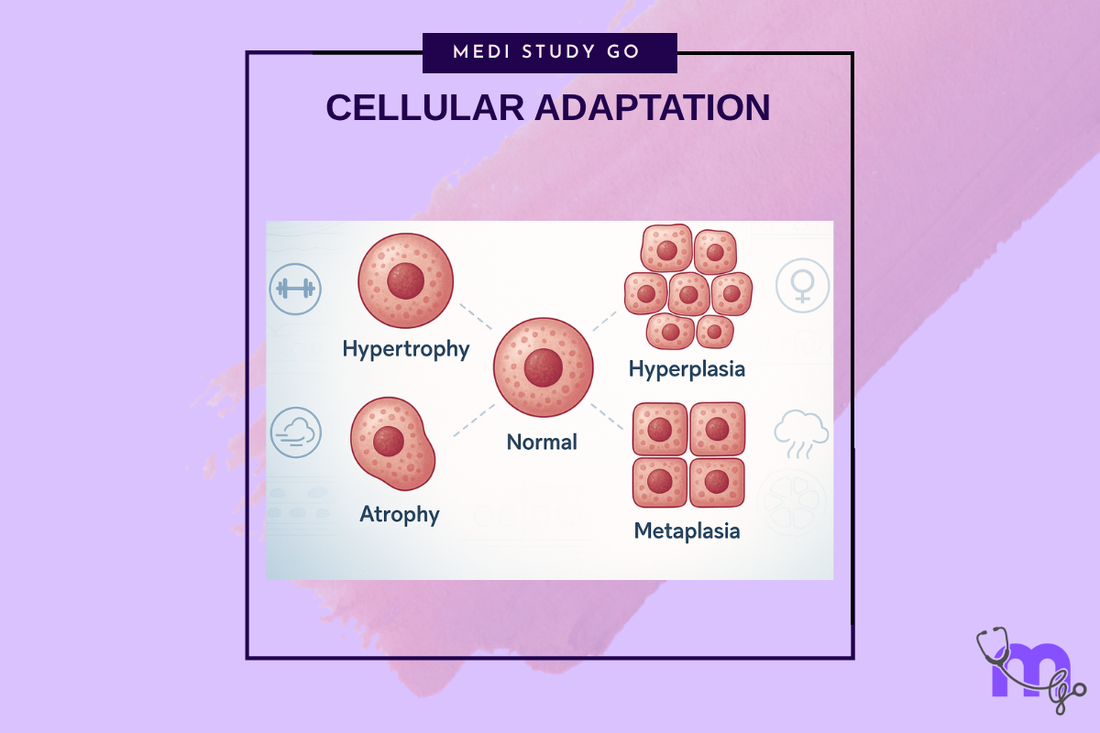
Related Resources
Cell Injury and Adaptation: The Foundation of Pathology
Morphology of Reversible Cell Injury: Key Features and Clinical Examples
Pathogenesis of Reversible Cell Injury: Mechanisms and Outcomes
Pathogenesis of Irreversible Cell Injury: From Damage to Cell Death
Necrosis: Types, Mechanisms, and Clinical Significance
Apoptosis: Programmed Cell Death in Health and Disease
Pathological Calcification: Dystrophic vs. Metastatic
Intracellular Accumulations: Lipids, Proteins, Pigments, and More
Cell Injury in Clinical Practice in Dentistry
Key Takeaways
- Cellular adaptation represents reversible changes that enable cells to survive and function under altered environmental conditions without injury
- The four main types of adaptation include hypertrophy (cell enlargement), hyperplasia (increased cell number), atrophy (cell shrinkage), and metaplasia (cell type transformation)
- Understanding adaptive responses helps distinguish normal physiological changes from pathological processes requiring intervention
- Recognition of adaptive patterns in oral tissues guides treatment decisions and helps predict tissue responses to therapeutic interventions
- Maladaptive responses can progress to cellular injury and disease, emphasizing the importance of monitoring adaptive changes over time
Introduction
Cellular adaptation represents the fundamental mechanism by which cells modify their structure, function, and metabolism to survive and maintain functionality under changing environmental conditions. For dental professionals, understanding cellular adaptation is essential for recognizing normal physiological responses, distinguishing adaptive changes from pathological processes, and predicting tissue responses to various stimuli and therapeutic interventions.
The adaptive response enables cells to achieve a new steady state that preserves viability and function while accommodating altered environmental demands. This process involves coordinated changes in gene expression, protein synthesis, organelle structure, and cellular metabolism that collectively enable cellular survival under conditions that might otherwise cause injury or death.
Cellular adaptation occurs in response to various stimuli including mechanical stress, altered functional demands, hormonal influences, nutritional changes, and chronic mild injury. The specific type of adaptive response depends on the nature of the stimulus, cellular capacity for adaptation, and duration of exposure to the altered conditions.
In dental practice, cellular adaptation is observed in numerous clinical situations including gingival response to plaque accumulation, pulpal response to caries or restorative procedures, periodontal ligament adaptation to orthodontic forces, and bone remodeling in response to functional demands. Understanding these processes enables better treatment planning and outcome prediction.
The clinical significance of cellular adaptation extends beyond recognition of normal responses to include identification of maladaptive changes that may progress to pathological conditions. Early recognition of inappropriate adaptive responses enables intervention to prevent progression to cellular injury and disease while optimizing therapeutic outcomes.
Table of Contents
Hypertrophy: Cellular Enlargement and Functional Enhancement What Drives Hyperplasia and When Does It Become Problematic? Atrophy: Cellular Shrinkage and Functional Decline How Does Metaplasia Represent Adaptive Cell Type Transformation? Clinical Recognition and Management of Adaptive Changes

Hypertrophy: Cellular Enlargement and Functional Enhancement
Mechanisms of Cellular Hypertrophy
Hypertrophy involves increase in cell size without increase in cell number, achieved through enhanced protein synthesis, organelle proliferation, and structural protein accumulation that enables cells to meet increased functional demands. This process requires coordinated upregulation of synthetic machinery and energy production systems.
The molecular mechanisms involve activation of growth factor signaling pathways, enhanced ribosomal biogenesis, increased mitochondrial number and function, and expansion of endoplasmic reticulum and other synthetic organelles. These changes collectively increase cellular capacity for work and metabolic activity.
Mechanical stress represents a primary stimulus for hypertrophy, particularly in muscle cells and connective tissue cells that experience increased functional demands. The mechanotransduction pathways convert physical forces into biochemical signals that regulate gene expression and cellular growth.
Physiological vs. Pathological Hypertrophy
Physiological hypertrophy occurs as a normal adaptive response to increased functional demands, such as muscle enlargement with exercise or glandular enlargement with increased secretory demands. This type of hypertrophy is beneficial and reversible when stimuli are removed.
Pathological hypertrophy develops in response to abnormal stimuli or when adaptive capacity is exceeded, potentially leading to cellular dysfunction and tissue damage. Examples include cardiac hypertrophy in response to hypertension or gingival hypertrophy from chronic inflammation.
The distinction between physiological and pathological hypertrophy is crucial for clinical management, as physiological hypertrophy typically requires no intervention while pathological hypertrophy may require treatment of underlying causes or direct therapeutic intervention.
Clinical Examples in Oral Tissues
Gingival hypertrophy represents a common adaptive response to chronic plaque accumulation, hormonal changes, or medication effects, involving increased cell size and enhanced inflammatory cell infiltration. Recognition of underlying causes guides appropriate treatment approaches.
Pulpal hypertrophy can occur in response to mild chronic irritation from caries or restorative procedures, involving increased odontoblast size and enhanced dentin production. Understanding this response helps predict pulpal treatment outcomes.
Masticatory muscle hypertrophy occurs in response to increased functional demands from bruxism or altered occlusion, potentially contributing to temporomandibular disorders. Recognition of this adaptation guides treatment planning for occlusal therapy.
What Drives Hyperplasia and When Does It Become Problematic?
Cellular Mechanisms of Hyperplasia
Hyperplasia involves increase in tissue size through increased cell number, achieved through enhanced cell proliferation that exceeds normal cell death rates. This process requires activation of cell cycle machinery and coordination with tissue organization mechanisms to maintain proper architecture.
Growth factor signaling plays crucial roles in hyperplastic responses, with various growth factors stimulating cell proliferation through specific signaling pathways. Understanding these pathways provides insights into therapeutic targets for managing excessive hyperplasia.
Cell cycle regulation in hyperplasia involves complex interactions between promoting and inhibiting factors that determine whether cells proceed through division cycles. Disruption of these regulatory mechanisms can lead to uncontrolled proliferation and neoplastic transformation.
Hormonal and Growth Factor Influences
Hormonal stimulation represents a major driver of hyperplastic responses, with estrogen, growth hormone, and other hormones promoting cell proliferation in target tissues. Understanding hormonal influences helps predict and manage hyperplastic responses in susceptible patients.
Growth factor availability and receptor expression determine cellular responsiveness to proliferative stimuli, with altered growth factor signaling contributing to both physiological and pathological hyperplasia. These mechanisms provide potential therapeutic targets.
The balance between proliferative stimuli and growth inhibitory factors determines the extent of hyperplastic response, with disruption of this balance potentially leading to excessive proliferation or neoplastic transformation.
Transition from Adaptive to Pathological
Physiological hyperplasia occurs as appropriate responses to normal stimuli such as hormonal changes during pregnancy or wound healing responses following injury. This type of hyperplasia is typically self-limited and beneficial.
Pathological hyperplasia involves excessive or inappropriate cell proliferation that may progress to neoplastic transformation if regulatory mechanisms become further disrupted. Recognition of this progression is crucial for early intervention.
Clinical monitoring of hyperplastic responses helps distinguish between appropriate adaptive changes and concerning proliferation that may require intervention. Understanding progression markers guides appropriate management decisions.
Oral Manifestations and Clinical Significance
Gingival hyperplasia can result from various causes including hormonal changes, medication effects, and chronic inflammation, with different underlying mechanisms requiring different treatment approaches. Recognition of causative factors guides therapeutic selection.
Inflammatory hyperplasia occurs in response to chronic irritation and represents attempts to cope with persistent stimuli. Examples include pyogenic granuloma and peripheral giant cell granuloma that require elimination of irritating factors.
Reactive hyperplasia develops in response to trauma or chronic irritation and may require surgical intervention if conservative measures fail to resolve the underlying causes. Understanding these conditions guides appropriate treatment sequencing.
Atrophy: Cellular Shrinkage and Functional Decline
Mechanisms of Cellular Atrophy
Atrophy involves decrease in cell size and number, achieved through reduced protein synthesis, increased protein degradation, decreased organelle number, and enhanced autophagy that collectively reduce cellular mass and metabolic activity. This process enables cellular survival under conditions of reduced nutrient availability or functional demand.
Autophagy plays crucial roles in atrophic responses by eliminating unnecessary cellular components and recycling materials for essential cellular functions. Understanding autophagy mechanisms provides insights into both physiological and pathological atrophy.
Protein degradation systems including ubiquitin-proteasome and lysosomal pathways become activated in atrophic responses, selectively degrading cellular proteins while preserving essential functions. The balance between synthesis and degradation determines the extent of atrophic change.
Causes and Clinical Patterns
Disuse atrophy occurs when tissues experience reduced functional demands, leading to adaptive reduction in cellular mass that reflects decreased metabolic requirements. This type is reversible with restoration of normal function.
Nutritional atrophy results from inadequate nutrient supply or impaired cellular uptake of essential nutrients, leading to cellular shrinkage as energy and building blocks become limiting. This pattern may indicate systemic or local nutritional deficiencies.
Hormonal atrophy occurs when hormonal support for cellular maintenance is withdrawn, leading to cellular shrinkage and functional decline. Understanding hormonal influences guides therapeutic approaches for hormone-dependent tissues.
Age-Related and Pathological Atrophy
Physiological atrophy occurs as part of normal aging processes and represents appropriate adaptation to changing functional demands and metabolic capacity. This type is generally gradual and associated with maintained function despite reduced tissue mass.
Pathological atrophy involves excessive or inappropriate cellular shrinkage that compromises tissue function and may indicate underlying disease processes. Recognition of pathological patterns guides appropriate diagnostic evaluation and intervention.
The distinction between physiological and pathological atrophy is important for clinical management, as pathological atrophy may require treatment while physiological atrophy typically requires only monitoring and supportive care.
Clinical Implications in Dental Practice
Alveolar bone atrophy following tooth loss represents a common adaptive response to reduced functional stimulation, with implications for prosthetic rehabilitation and implant placement. Understanding remodeling patterns guides treatment planning.
Gingival atrophy can occur with aging or following periodontal therapy, potentially exposing root surfaces and affecting esthetics. Recognition of risk factors enables preventive strategies and appropriate management.
Salivary gland atrophy may occur with aging, medications, or systemic diseases, affecting oral health through reduced salivary flow. Understanding these relationships guides diagnostic evaluation and management strategies.
How Does Metaplasia Represent Adaptive Cell Type Transformation?
Cellular Mechanisms of Metaplasia
Metaplasia involves replacement of one differentiated cell type with another mature differentiated cell type, typically representing adaptation to chronic irritation or altered environmental conditions. This process involves reprogramming of cellular differentiation pathways rather than simple cellular injury.
Stem cell activation and altered differentiation patterns drive metaplastic responses, with uncommitted stem cells differentiating into cell types better adapted to prevailing environmental conditions. Understanding stem cell biology provides insights into metaplastic mechanisms.
Transcriptional reprogramming underlies metaplastic transformation, involving changes in gene expression patterns that redirect cellular differentiation toward more appropriate cell types for existing environmental conditions.
Types and Clinical Examples
Squamous metaplasia involves replacement of other epithelial cell types with squamous epithelium, typically occurring in response to chronic irritation or inflammation. This transformation provides enhanced protection against mechanical or chemical trauma.
Respiratory epithelium metaplasia can occur in oral tissues exposed to chronic irritation, with ciliated respiratory epithelium replacing normal oral epithelium in some circumstances. Recognition of this change guides identification of underlying irritants.
Intestinal metaplasia may occur in gastric tissue but can occasionally be observed in oral tissues under specific circumstances, representing adaptation to altered chemical environments.
Adaptive vs. Dysplastic Changes
Metaplasia represents organized adaptive responses with maintained cellular organization and function, whereas dysplasia involves disorganized cellular changes that may progress to neoplastic transformation. Distinguishing between these patterns is crucial for appropriate management.
The reversibility of metaplastic changes depends on elimination of underlying stimuli, with most metaplastic responses being reversible when irritating factors are removed. This reversibility distinguishes metaplasia from neoplastic transformation.
Monitoring metaplastic changes helps identify progression toward dysplasia or neoplasia, enabling early intervention when concerning changes develop. Understanding progression markers guides appropriate follow-up protocols.
Clinical Recognition and Management
Chronic irritation identification represents the key to managing metaplastic responses, as elimination of irritating stimuli typically leads to reversal of metaplastic changes. Systematic evaluation for sources of chronic irritation guides therapeutic approaches.
Biopsy evaluation may be necessary to distinguish metaplastic changes from dysplastic or neoplastic processes, particularly when clinical appearance is concerning or when metaplastic changes persist despite elimination of apparent irritants.
Long-term monitoring of metaplastic areas ensures appropriate recognition of changes that might indicate progression toward more serious pathological processes requiring additional intervention.
Clinical Recognition and Management of Adaptive Changes
Assessment and Diagnosis
Clinical evaluation of adaptive changes requires understanding of normal tissue architecture and function to distinguish adaptive responses from pathological processes. Systematic examination techniques enable recognition of subtle adaptive changes.
History taking should focus on identifying potential stimuli for adaptive responses including functional changes, environmental exposures, medications, and systemic conditions that might influence cellular adaptation patterns.
Radiographic evaluation may reveal structural changes associated with adaptive responses, particularly in bone and other mineralized tissues where adaptive remodeling can be visualized through imaging studies.
Monitoring and Follow-up
Serial evaluation enables assessment of adaptive change progression and response to therapeutic interventions, helping distinguish between appropriate adaptive responses and concerning changes requiring intervention.
Documentation of adaptive changes provides baseline information for future comparison and enables recognition of progression or improvement over time. Standardized documentation approaches enhance monitoring effectiveness.
Patient education regarding adaptive changes helps ensure compliance with monitoring protocols and enables patients to recognize concerning changes that might require earlier evaluation.
Therapeutic Approaches
Stimulus modification represents the primary approach for managing adaptive responses, involving identification and elimination or modification of factors driving adaptive changes. This approach addresses underlying causes rather than simply treating symptoms.
Supportive therapy may be appropriate for physiological adaptive responses that do not require intervention but benefit from optimization of healing conditions and prevention of complications.
Intervention timing is crucial for managing adaptive responses, with early intervention typically being more effective than delayed treatment after adaptive changes have become established or progressed to pathological states.
Prevention Strategies
Risk factor identification enables implementation of preventive strategies that minimize the likelihood of maladaptive responses while supporting appropriate physiological adaptation to changing conditions.
Environmental modification can prevent or minimize stimuli that drive unwanted adaptive responses, emphasizing the importance of comprehensive assessment of patient environmental and lifestyle factors.
Patient counseling regarding factors that influence adaptive responses enhances prevention effectiveness and supports patient participation in maintaining optimal oral health through appropriate adaptation management.
Conclusion
Understanding cellular adaptation mechanisms and their clinical manifestations provides essential knowledge for recognizing normal physiological responses, distinguishing adaptive changes from pathological processes, and implementing appropriate management strategies that support beneficial adaptation while preventing maladaptive responses.
The recognition that adaptive changes can be either beneficial or harmful emphasizes the importance of comprehensive assessment that considers underlying causes, patient factors, and potential for progression to pathological states. This understanding guides appropriate intervention decisions and monitoring protocols.
Clinical applications of adaptation principles continue to evolve with advancing understanding of cellular and molecular mechanisms, providing opportunities for more precise therapeutic approaches that optimize adaptive responses while minimizing unwanted consequences.
The integration of cellular adaptation concepts with clinical practice represents a fundamental aspect of dental medicine that influences treatment planning, outcome prediction, and long-term patient management strategies across all aspects of oral healthcare.