Morphology of Reversible Cell Injury: Key Features and Clinical Examples
Medi Study Go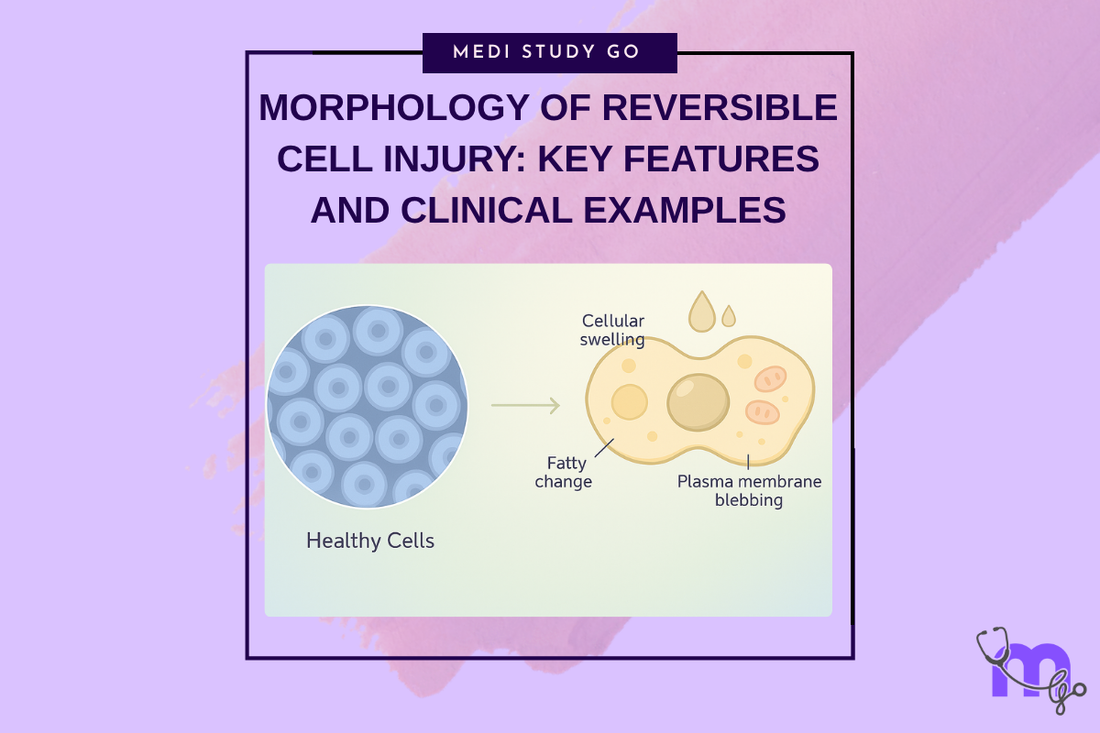
Related Resources
Cell Injury and Adaptation: The Foundation of Pathology
Pathogenesis of Reversible Cell Injury: Mechanisms and Outcomes
Pathogenesis of Irreversible Cell Injury: From Damage to Cell Death
Necrosis: Types, Mechanisms, and Clinical Significance
Apoptosis: Programmed Cell Death in Health and Disease
Pathological Calcification: Dystrophic vs. Metastatic
Cellular Adaptation: Types, Mechanisms, and Clinical Relevance
Intracellular Accumulations: Lipids, Proteins, Pigments, and More
Cell Injury in Clinical Practice in Dentistry
Key Takeaways
- Cellular swelling represents the earliest and most common manifestation of reversible cell injury, resulting from ATP depletion and Na+/K+ pump dysfunction
- Fatty change occurs predominantly in liver and heart tissues, involving accumulation of triglycerides within cytoplasm due to altered fatty acid metabolism
- Recognition of reversible injury morphology enables early intervention to prevent progression to irreversible cellular damage
- Microscopic features including cytoplasmic blebs, mitochondrial swelling, and small densities indicate cellular stress before irreversible changes occur
- Understanding morphological patterns helps dental professionals distinguish between reversible and irreversible tissue damage in clinical practice
Introduction
The morphological features of reversible cell injury represent critical diagnostic markers that enable dental professionals to recognize early cellular damage and implement appropriate interventions before progression to irreversible tissue loss. Understanding these morphological changes provides the foundation for distinguishing between conditions that can be successfully treated and those requiring more aggressive therapeutic approaches.
Reversible cell injury manifests through characteristic structural alterations that reflect underlying metabolic disturbances while maintaining the potential for complete recovery when the injurious stimulus is removed. These changes occur in a predictable sequence, beginning with functional alterations that progress to visible morphological modifications observable through various diagnostic techniques.
In dental practice, recognizing reversible injury morphology is essential for managing conditions such as pulpal inflammation, periodontal tissue damage, and post-surgical healing complications. Early identification of these changes allows practitioners to modify treatment approaches, optimize healing conditions, and prevent progression to irreversible injury requiring more extensive interventions.
The clinical significance of understanding reversible injury morphology extends beyond immediate treatment decisions to include long-term tissue preservation strategies and patient education regarding risk factors. Modern diagnostic techniques including histopathological examination, advanced imaging, and biomarker analysis provide detailed information about cellular morphology that directly influences treatment planning and prognosis assessment.
Contemporary research in cellular pathology continues to refine our understanding of reversible injury patterns, with particular emphasis on identifying early markers that predict treatment response and tissue recovery potential. These advances enable more precise diagnostic approaches and targeted therapeutic interventions that optimize patient outcomes while minimizing treatment complexity and cost.
Table of Contents
Understanding Cellular Swelling in Oral Tissues
What Are the Key Microscopic Features of Reversible Cell Injury?
Fatty Change: Mechanisms and Clinical Relevance
How Do Morphological Changes Progress in Reversible Injury?
Clinical Recognition and Diagnostic Applications
Understanding Cellular Swelling in Oral Tissues

Pathophysiological Basis of Cellular Swelling
Cellular swelling occurs as the earliest and most universal response to cellular injury, resulting from disruption of normal cellular energy metabolism and subsequent failure of ATP-dependent ion transport mechanisms. When cellular ATP levels decrease due to hypoxia, toxin exposure, or other injurious stimuli, the Na+/K+ ATPase pump becomes inactive, leading to sodium accumulation within cells and subsequent water influx to maintain osmotic equilibrium.
This process affects all cellular compartments but is most readily observable in the cytoplasm, where accumulation of intracellular water creates the characteristic appearance of enlarged, pale-staining cells. The endoplasmic reticulum and mitochondria also demonstrate swelling, contributing to overall cellular enlargement and altered cellular architecture that can be detected through various diagnostic modalities.
The reversible nature of cellular swelling depends on restoration of normal ATP production and ion pump function. When the underlying cause is addressed promptly, cells can rapidly restore normal volume and function through active transport mechanisms that eliminate excess sodium and water. However, prolonged swelling can progress to irreversible injury if cellular energy metabolism cannot be restored.
Clinical Manifestations in Dental Practice
In oral tissues, cellular swelling manifests as tissue edema, altered tissue consistency, and modified healing responses that can be observed clinically. Gingival tissues may appear enlarged and spongy, while pulpal tissues demonstrate increased pressure and altered vascular dynamics that affect pain perception and treatment response.
Post-surgical cellular swelling represents a normal response to tissue trauma but requires monitoring to distinguish between physiological healing responses and pathological progression. Understanding the timeline and characteristics of normal cellular swelling helps practitioners recognize when intervention is necessary to prevent complications.
Chronic cellular swelling can indicate ongoing tissue stress that may progress to more serious pathological changes if underlying causes are not addressed. This is particularly relevant in periodontal disease where persistent inflammation can lead to sustained cellular swelling and eventual tissue destruction.
What Are the Key Microscopic Features of Reversible Cell Injury?
Reversible cell injury demonstrates characteristic microscopic features that distinguish it from normal cellular architecture while maintaining potential for complete recovery. These features include cytoplasmic blebs, mitochondrial changes, and alterations in cellular organelles that reflect underlying metabolic disturbances without permanent structural damage.
Cytoplasmic and Membrane Changes
Cytoplasmic blebs represent focal protrusions of the cell membrane that occur due to altered membrane integrity and cytoskeletal organization. These structures indicate cellular stress but remain reversible when normal cellular function is restored. The presence of blebs often correlates with the severity of injury and can serve as an early indicator of cellular dysfunction.
Loss of microvilli represents another significant morphological change in reversible injury, particularly relevant in epithelial tissues where these structures are essential for absorption and secretory functions. This change affects cellular function but can be completely restored when normal cellular metabolism is reestablished.
Endoplasmic reticulum swelling and ribosomal detachment indicate disruption of protein synthesis machinery, leading to decreased protein production and altered cellular function. These changes are completely reversible and represent adaptive responses to cellular stress rather than permanent structural damage.
Mitochondrial Alterations
Mitochondrial swelling with small densities represents one of the earliest ultrastructural changes in reversible cell injury. These organelles demonstrate altered internal architecture while maintaining basic structural integrity and potential for functional recovery. The appearance of small densities within mitochondria indicates altered calcium homeostasis but does not represent irreversible damage.
The distinction between small and large mitochondrial densities is crucial for determining injury reversibility. Small densities indicate reversible changes that can be corrected through restoration of normal cellular metabolism, while large amorphous densities suggest progression to irreversible injury requiring different therapeutic approaches.
Fatty Change: Mechanisms and Clinical Relevance
Understanding Fatty Change Pathophysiology
Fatty change involves accumulation of triglycerides within cellular cytoplasm due to altered fatty acid metabolism, most commonly observed in liver and heart tissues but with systemic implications relevant to dental practice. This process occurs when cellular uptake of fatty acids exceeds the cell's capacity for fatty acid oxidation or export, leading to triglyceride accumulation in cytoplasmic vacuoles.
The mechanism involves disruption of normal fatty acid metabolism through several pathways including increased fatty acid synthesis, decreased fatty acid oxidation, impaired protein synthesis affecting lipoprotein formation, and altered membrane transport mechanisms. These changes can result from hypoxia, toxin exposure, nutritional imbalances, or hormonal disturbances.
Fatty change is completely reversible when the underlying metabolic disturbance is corrected, making early recognition and intervention crucial for preventing progression to more serious pathological changes. The process of resolution involves restoration of normal fatty acid metabolism and clearance of accumulated triglycerides through enhanced oxidation and export mechanisms.
Clinical Implications in Dental Practice
While fatty change primarily affects liver and cardiac tissues, understanding this process is relevant to dental practice due to systemic health connections and potential medication-related complications. Patients with hepatic fatty change may demonstrate altered drug metabolism affecting anesthetic and analgesic responses during dental procedures.
The systemic inflammatory response associated with fatty change can influence oral tissue healing and susceptibility to infection, requiring modified treatment approaches and enhanced monitoring during dental interventions. Recognition of patients at risk for fatty change enables practitioners to adjust treatment protocols and coordinate care with medical colleagues.
Alcohol-related fatty change represents a particular concern in dental practice due to the high prevalence of alcohol use disorders and associated oral health complications. Understanding the relationship between fatty change and systemic health enables practitioners to provide comprehensive care while addressing underlying risk factors.
How Do Morphological Changes Progress in Reversible Injury?
The progression of morphological changes in reversible cell injury follows a predictable sequence that reflects the underlying pathophysiological processes and cellular adaptive responses. Understanding this progression enables practitioners to assess injury severity, predict treatment response, and implement appropriate interventions at optimal timing.
Early Morphological Changes
Initial changes include functional alterations that precede visible morphological modifications, including decreased enzyme activity, altered membrane permeability, and modified ion transport mechanisms. These changes can be detected through biochemical analysis before structural alterations become apparent through microscopic examination.
The earliest visible changes involve cellular swelling and organelle modifications that indicate metabolic dysfunction while maintaining cellular viability. Mitochondrial swelling with small densities, endoplasmic reticulum dilation, and ribosomal detachment represent early markers of cellular stress that remain completely reversible with appropriate intervention.
Membrane changes including loss of microvilli and formation of cytoplasmic blebs indicate more advanced cellular dysfunction but still maintain potential for complete recovery. These changes affect cellular function and require prompt intervention to prevent progression to irreversible injury.
Transition Points and Recovery Potential
The transition from early to advanced reversible injury involves more pronounced morphological changes including increased cellular swelling, more extensive organelle modifications, and altered nuclear morphology. However, these changes remain reversible if underlying causes are addressed promptly and appropriately.
Recovery from reversible injury involves restoration of normal cellular morphology through correction of underlying metabolic disturbances and restoration of normal cellular function. The timeline for morphological recovery varies depending on injury severity, underlying cause, and effectiveness of therapeutic interventions.
Recognition of transition points between reversible and irreversible injury is crucial for treatment planning and prognosis assessment. Understanding the morphological features that indicate potential for recovery versus progression to cell death enables practitioners to make informed decisions regarding treatment intensity and patient expectations.
Clinical Recognition and Diagnostic Applications
Diagnostic Techniques for Morphological Assessment
Clinical recognition of reversible injury morphology requires integration of multiple diagnostic approaches including histopathological examination, imaging studies, and functional assessments. Light microscopy provides basic morphological information while electron microscopy offers detailed ultrastructural analysis for precise characterization of cellular changes.
Advanced imaging techniques including confocal microscopy and specialized staining methods enable real-time assessment of cellular morphology and function, providing valuable information for treatment planning and monitoring. These techniques are particularly useful for research applications and complex clinical cases requiring detailed morphological analysis.
Biomarker analysis complements morphological assessment by providing functional information about cellular metabolism and injury severity. Integration of morphological and biochemical data enables comprehensive assessment of cellular injury and recovery potential.
Clinical Applications and Treatment Implications
Recognition of reversible injury morphology directly influences treatment decisions including intervention timing, therapy selection, and monitoring protocols. Early recognition enables implementation of supportive measures that optimize cellular recovery while preventing progression to irreversible injury.
Patient education regarding morphological changes and recovery potential enhances compliance with treatment recommendations and supports optimal outcomes. Understanding the relationship between morphological changes and functional recovery helps patients develop realistic expectations regarding treatment timelines and outcomes.
Long-term monitoring of morphological recovery provides valuable information for assessing treatment effectiveness and identifying patients at risk for recurrent injury. This information supports development of individualized prevention strategies and long-term care planning.
Conclusion
Understanding the morphology of reversible cell injury provides essential knowledge for recognizing early cellular damage and implementing appropriate therapeutic interventions in dental practice. The characteristic features of cellular swelling, fatty change, and organelle modifications represent valuable diagnostic markers that enable distinction between reversible and irreversible tissue damage.
Recognition of these morphological patterns requires integration of clinical observation, diagnostic testing, and understanding of underlying pathophysiological processes. Early identification of reversible injury features enables prompt intervention that can prevent progression to irreversible damage and optimize patient outcomes.
The clinical applications of morphological assessment extend beyond immediate treatment decisions to include long-term tissue preservation strategies, patient education, and development of individualized care plans. Contemporary diagnostic techniques continue to enhance our ability to recognize and characterize reversible injury patterns with increasing precision and clinical relevance.
Future developments in cellular imaging and analysis promise to provide even more detailed information about reversible injury morphology, enabling more targeted therapeutic approaches and improved patient outcomes. The integration of morphological assessment with functional evaluation and molecular analysis represents the future of personalized medicine in dental practice.