Pathogenesis of Reversible Cell Injury: Mechanisms and Outcomes
Medi Study Go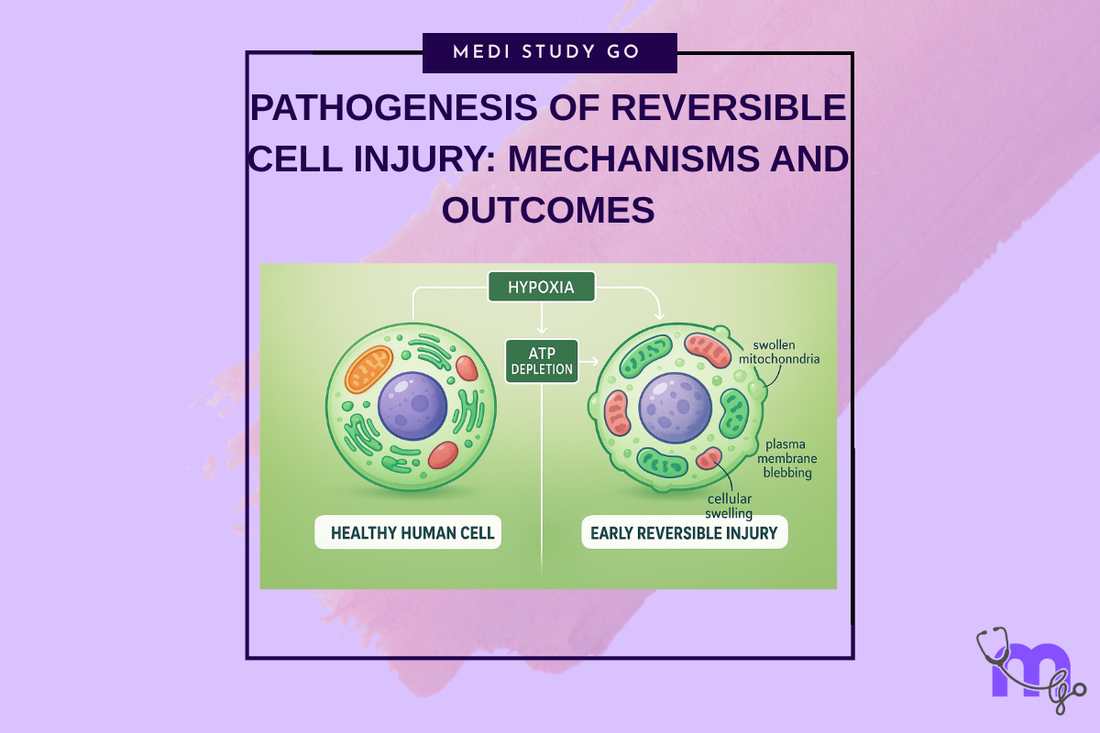
Related Resources
Cell Injury and Adaptation: The Foundation of Pathology
Morphology of Reversible Cell Injury: Key Features and Clinical Examples
Pathogenesis of Irreversible Cell Injury: From Damage to Cell Death
Necrosis: Types, Mechanisms, and Clinical Significance
Apoptosis: Programmed Cell Death in Health and Disease
Pathological Calcification: Dystrophic vs. Metastatic
Cellular Adaptation: Types, Mechanisms, and Clinical Relevance
Intracellular Accumulations: Lipids, Proteins, Pigments, and More
Cell Injury in Clinical Practice in Dentistry
Key Takeaways
- Hypoxia-induced ATP depletion represents the primary mechanism initiating reversible cell injury through disruption of energy-dependent cellular processes
- Membrane dysfunction resulting from ion pump failure leads to cellular swelling and altered cellular homeostasis that characterizes early injury responses
- Calcium homeostasis disruption activates destructive enzymes including phospholipases, proteases, and endonucleases that can progress injury toward irreversibility
- Understanding these mechanisms enables targeted therapeutic interventions that support cellular recovery and prevent progression to irreversible damage
- Recognition of pathogenetic pathways guides clinical decision-making regarding treatment timing, intervention selection, and patient monitoring protocols
Introduction
The pathogenesis of reversible cell injury encompasses a complex cascade of molecular and cellular events that determine whether tissues can recover from injurious stimuli or progress to irreversible damage and cell death. Understanding these pathogenetic mechanisms is fundamental for dental professionals who regularly encounter tissues affected by hypoxia, inflammation, trauma, and chemical exposure that can trigger cellular injury responses.
The sequence of events in reversible cell injury begins with disruption of normal cellular energy metabolism, leading to a cascade of biochemical alterations that affect multiple cellular systems. The early changes involve ATP depletion, ion pump dysfunction, and altered membrane integrity that create the characteristic morphological and functional changes associated with reversible injury.
Critical to understanding reversible injury pathogenesis is recognition that these processes remain potentially reversible until specific threshold points are reached. The distinction between reversible and irreversible injury depends on the severity and duration of the injurious stimulus, the cellular adaptive capacity, and the effectiveness of therapeutic interventions implemented during the reversible phase.
In dental practice, reversible cell injury pathogenesis is particularly relevant in conditions such as pulpal inflammation, periodontal tissue damage, post-surgical healing complications, and responses to dental materials. Understanding the underlying mechanisms enables practitioners to recognize early injury signs, implement appropriate interventions, and optimize conditions for cellular recovery.
Contemporary research continues to elucidate the molecular mechanisms underlying reversible cell injury, with particular focus on cellular signaling pathways, metabolic adaptations, and therapeutic targets that can enhance cellular recovery. These advances provide new opportunities for more precise diagnostic approaches and targeted therapeutic interventions that improve patient outcomes while reducing treatment complexity.
Table of Contents
Hypoxia and ATP Depletion: The Primary Trigger What Role Does Membrane Dysfunction Play in Reversible Injury? Calcium Homeostasis and Enzyme Activation How Do Cellular Organelles Respond to Injury? Molecular Mechanisms and Recovery Pathways

Hypoxia and ATP Depletion: The Primary Trigger
Cellular Energy Metabolism Disruption
Hypoxia represents the most common initiating factor in reversible cell injury, occurring when tissue oxygen supply becomes inadequate to meet cellular metabolic demands. This condition triggers a cascade of metabolic alterations beginning with impaired oxidative phosphorylation in mitochondria, leading to decreased ATP production and activation of anaerobic glycolysis as a compensatory mechanism.
The shift from aerobic to anaerobic metabolism results in several critical changes including decreased ATP availability for essential cellular processes, increased lactate production leading to cellular acidosis, and depletion of cellular energy stores that compromises multiple cellular functions. These changes occur rapidly following oxygen deprivation and represent the earliest pathogenetic events in reversible cell injury.
ATP depletion affects numerous cellular processes simultaneously, including active transport mechanisms, protein synthesis, DNA repair, and maintenance of cellular structure. The severity of these effects depends on the degree and duration of ATP depletion, with mild reductions causing functional impairment while severe depletion can progress to irreversible cellular damage.
Consequences of Energy Failure
Na+/K+ ATPase pump dysfunction represents one of the earliest and most significant consequences of ATP depletion, leading to loss of normal ion gradients across cellular membranes. This results in sodium accumulation within cells, potassium loss, and subsequent water influx that creates the characteristic cellular swelling observed in reversible injury.
Protein synthesis inhibition occurs due to energy requirements for ribosomal function and amino acid transport. This leads to decreased production of essential cellular proteins including enzymes, structural proteins, and transport proteins that are necessary for normal cellular function and recovery from injury.
Calcium pump dysfunction represents another critical consequence of ATP depletion, leading to disruption of normal calcium homeostasis and potential activation of calcium-dependent destructive enzymes. Understanding these consequences enables practitioners to implement interventions that support cellular energy metabolism and prevent progression to irreversible injury.
Recovery Mechanisms and Therapeutic Implications
Recovery from hypoxia-induced ATP depletion requires restoration of adequate oxygen supply and correction of underlying metabolic disturbances. This involves improving tissue perfusion, eliminating injurious stimuli, and supporting cellular metabolic processes through appropriate therapeutic interventions.
The timeline for recovery depends on the severity and duration of hypoxia, with brief episodes causing minimal lasting effects while prolonged hypoxia can result in accumulated cellular damage that requires extended recovery periods. Understanding these timelines helps practitioners develop realistic treatment expectations and monitoring protocols.
Therapeutic approaches that support cellular energy metabolism include maintaining adequate tissue oxygenation, optimizing nutritional status, and using medications that support mitochondrial function. These interventions can significantly enhance recovery from reversible injury and prevent progression to irreversible damage.
What Role Does Membrane Dysfunction Play in Reversible Injury?
Membrane dysfunction represents a central mechanism in reversible cell injury pathogenesis, affecting cellular integrity, ion homeostasis, and communication between cellular compartments. This dysfunction results from both direct membrane damage and secondary effects of metabolic disturbances that compromise membrane structure and function.
Ion Transport Disruption
The failure of ATP-dependent ion transport systems, particularly the Na+/K+ ATPase pump, creates profound alterations in cellular ion homeostasis that characterize reversible injury. Normal cellular function depends on maintenance of specific ion gradients across membranes, with disruption of these gradients leading to cellular dysfunction and morphological changes.
Sodium accumulation within cells occurs when the Na+/K+ pump cannot maintain normal ion gradients, leading to osmotic changes that draw water into cells and create characteristic cellular swelling. This process affects all cellular compartments and can significantly alter cellular function while remaining potentially reversible with restoration of normal pump function.
Potassium loss from cells accompanies sodium accumulation and contributes to altered cellular excitability and function. This is particularly significant in excitable tissues such as nerve and muscle where potassium gradients are essential for normal electrical activity and cellular communication.
Membrane Integrity and Permeability Changes
Altered membrane permeability occurs due to both direct membrane damage and secondary effects of metabolic disturbances. These changes allow inappropriate movement of ions and molecules across membranes, contributing to cellular dysfunction and progression of injury processes.
Loss of membrane selectivity represents a critical aspect of membrane dysfunction, allowing substances that are normally excluded from cells to enter and essential cellular components to leak out. This process contributes to cellular dysfunction and can indicate progression toward irreversible injury if not corrected promptly.
Formation of cytoplasmic blebs and membrane protrusions indicates severe membrane dysfunction while often remaining reversible with appropriate intervention. These morphological changes reflect underlying membrane instability and require prompt attention to prevent progression to irreversible membrane damage.
Recovery and Therapeutic Considerations
Membrane recovery requires restoration of normal cellular energy metabolism and correction of underlying factors contributing to membrane dysfunction. This involves addressing hypoxia, eliminating toxic substances, and supporting cellular repair mechanisms that can restore normal membrane structure and function.
The potential for membrane recovery depends on the extent of damage and the duration of dysfunction. Early intervention during the reversible phase can lead to complete restoration of normal membrane function, while delayed intervention may result in irreversible membrane damage requiring more extensive therapeutic approaches.
Calcium Homeostasis and Enzyme Activation
Disruption of Calcium Regulation
Calcium homeostasis disruption represents a critical pathogenetic mechanism in reversible cell injury that can determine whether cells recover or progress to irreversible damage. Normal cellular function requires precise regulation of intracellular calcium concentrations, with disruption of this regulation leading to activation of destructive cellular processes.
ATP depletion impairs calcium pump function in both the endoplasmic reticulum and cell membrane, leading to increased cytosolic calcium concentrations. This increase can activate numerous calcium-dependent enzymes that can damage cellular structures and contribute to progression from reversible to irreversible injury.
The sources of increased intracellular calcium include release from intracellular stores due to pump dysfunction, increased membrane permeability allowing calcium influx, and decreased calcium extrusion due to energy depletion. Understanding these sources enables targeted therapeutic approaches to maintain calcium homeostasis during cellular injury.
Enzyme Activation and Cellular Damage
Phospholipase activation due to increased intracellular calcium leads to membrane phospholipid breakdown, contributing to membrane dysfunction and altered cellular permeability. This process can create a positive feedback loop where membrane damage leads to further calcium influx and additional enzyme activation.
Protease activation results in breakdown of cellular proteins including structural proteins, enzymes, and transport proteins essential for normal cellular function. This process contributes to cellular dysfunction and can indicate progression from reversible to irreversible injury depending on the extent of protein damage.
Endonuclease activation leads to DNA fragmentation that can compromise cellular function and viability. While limited DNA damage may be repairable, extensive endonuclease activation can result in irreversible cellular damage requiring more aggressive therapeutic interventions.
Therapeutic Targeting of Calcium Pathways
Calcium channel blockers and calcium-binding agents represent potential therapeutic approaches for managing reversible cell injury by preventing excessive calcium accumulation and enzyme activation. These interventions can be particularly valuable in conditions where calcium homeostasis disruption is a primary pathogenetic mechanism.
Restoration of cellular energy metabolism represents the most effective approach for correcting calcium homeostasis disruption by restoring normal pump function and cellular calcium regulation. This emphasizes the importance of addressing underlying causes of ATP depletion in reversible cell injury.
How Do Cellular Organelles Respond to Injury?
Cellular organelles demonstrate characteristic responses to injury that reflect their specific functions and vulnerability to various injurious stimuli. Understanding these responses enables recognition of injury patterns and assessment of recovery potential in clinical practice.
Mitochondrial Responses
Mitochondrial swelling represents one of the earliest ultrastructural changes in reversible cell injury, reflecting altered membrane permeability and ion homeostasis within these organelles. The appearance of small densities within mitochondria indicates calcium accumulation but remains reversible with restoration of normal cellular metabolism.
Oxidative phosphorylation dysfunction occurs early in hypoxic injury and directly contributes to ATP depletion that characterizes reversible injury. This dysfunction affects the electron transport chain and ATP synthesis, leading to the metabolic consequences that define reversible cell injury pathogenesis.
Recovery of mitochondrial function requires restoration of adequate oxygen supply and correction of metabolic disturbances that impair oxidative phosphorylation. The potential for complete functional recovery makes early intervention crucial for optimizing outcomes in reversible cell injury.
Endoplasmic Reticulum and Protein Synthesis
Endoplasmic reticulum swelling and ribosomal detachment occur due to altered cellular energy metabolism and ion homeostasis, leading to impaired protein synthesis that affects cellular function and recovery potential. These changes are completely reversible with restoration of normal cellular conditions.
Decreased protein synthesis affects production of enzymes, structural proteins, and transport proteins essential for cellular function and recovery from injury. Understanding this mechanism emphasizes the importance of supporting cellular metabolic processes during recovery from reversible injury.
The relationship between protein synthesis recovery and overall cellular recovery makes monitoring of protein synthesis markers valuable for assessing treatment effectiveness and predicting outcomes in reversible cell injury.
Nuclear and Cytoskeletal Responses
Chromatin clumping represents an early nuclear response to cellular injury that reflects altered ionic conditions and metabolic disturbances. This change is reversible and indicates cellular stress without permanent nuclear damage.
Cytoskeletal alterations contribute to morphological changes including cytoplasmic blebbing and altered cellular shape that characterize reversible injury. These changes affect cellular function but remain reversible with correction of underlying metabolic disturbances.
Molecular Mechanisms and Recovery Pathways
Cellular Signaling in Injury and Recovery
Cellular signaling pathways play crucial roles in both injury development and recovery processes, with specific pathways activated in response to various injurious stimuli. Understanding these pathways enables targeted therapeutic approaches that can enhance recovery and prevent progression to irreversible injury.
Stress response pathways including heat shock protein production and antioxidant enzyme activation represent important cellular defense mechanisms that can be enhanced through appropriate therapeutic interventions. These pathways help cells survive injurious conditions and recover normal function.
Growth factor signaling and cellular repair pathways become activated during recovery from reversible injury, promoting restoration of normal cellular structure and function. Supporting these pathways through appropriate growth factors and nutrients can enhance recovery outcomes.
Therapeutic Targets and Recovery Enhancement
Antioxidant therapy represents an important approach for managing reversible cell injury by reducing oxidative stress and supporting cellular defense mechanisms. This is particularly relevant in conditions where free radical generation contributes to cellular injury.
Metabolic support through appropriate nutrition, oxygen therapy, and medications that support cellular energy metabolism can significantly enhance recovery from reversible cell injury. These approaches address the fundamental mechanisms underlying injury pathogenesis.
Anti-inflammatory interventions can help manage secondary inflammatory responses that can contribute to progression of cellular injury. Understanding the balance between beneficial and harmful inflammatory responses guides appropriate therapeutic approaches.
Conclusion
Understanding the pathogenesis of reversible cell injury provides essential knowledge for recognizing injury mechanisms, predicting outcomes, and implementing appropriate therapeutic interventions in dental practice. The complex cascade of events involving ATP depletion, membrane dysfunction, calcium homeostasis disruption, and organelle responses determines whether cells can recover or progress to irreversible damage.
Recognition of these pathogenetic mechanisms enables targeted therapeutic approaches that address underlying causes rather than simply treating symptoms. Early intervention during the reversible phase can lead to complete cellular recovery, while delayed intervention may result in progression to irreversible injury requiring more extensive treatment.
The clinical applications of understanding reversible injury pathogenesis extend to treatment planning, patient monitoring, and development of prevention strategies that minimize cellular injury risk. Contemporary research continues to identify new therapeutic targets and approaches that can enhance cellular recovery and improve patient outcomes.
Future developments in cellular therapy and regenerative medicine promise to provide even more effective interventions for managing reversible cell injury. The integration of molecular understanding with clinical practice represents the foundation for advancing dental medicine toward more precise and effective therapeutic approaches.