Torus Removal in Pre-Prosthetic Surgery: Indications, Surgical Steps, and Complications
Medi Study Go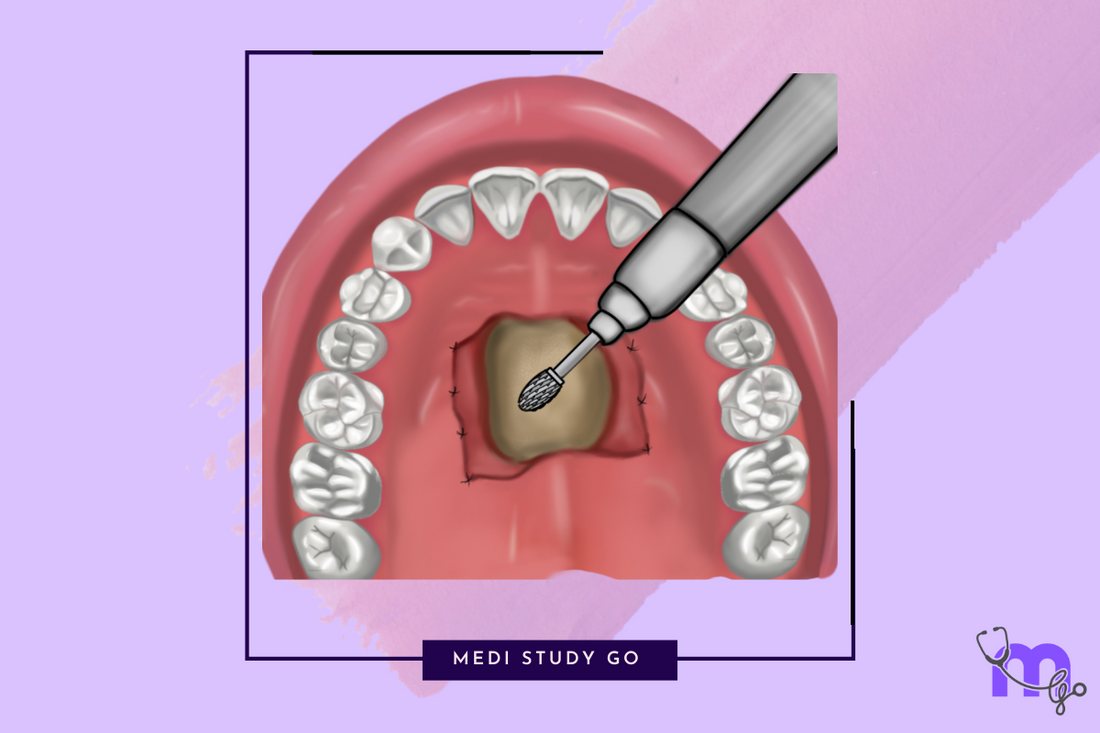
Related Resources:
- Comprehensive Guide to Pre-Prosthetic Surgery: Techniques, Indications, and Clinical Relevance for Dental Students
- Alveolar Ridge Correction in Pre-Prosthetic Surgery: Methods, Indications, and Exam-Focused Insights
- Alveoloplasty: Procedure, Clinical Applications, and Key Points
- Vestibuloplasty Techniques: Comparative Review and Clinical Decision-Making
- Ridge Augmentation and Frenectomy: Modern Approaches and Evidence-Based Outcomes
Key Takeaways:
- Tori represent benign bony outgrowths that may interfere with denture fabrication and stability
- Removal is primarily indicated for prosthetic considerations in edentulous patients
- Specific surgical techniques exist for both palatine and lingual tori
- Careful attention to anatomical structures prevents major complications
- Proper case selection and patient preparation are essential for successful outcomes
Introduction
Tori represent innocuous bony outgrowths that, while typically asymptomatic in dentate individuals, can present significant challenges during prosthetic rehabilitation of the edentulous patient. These benign osseous proliferations, most commonly presenting as torus palatinus in the maxilla and torus mandibularis (lingual tori) in the mandible, frequently interfere with denture fabrication, adaptation, and function, necessitating their removal as part of comprehensive pre-prosthetic preparation.
For dental students and practitioners involved in prosthetic rehabilitation, understanding the indications, techniques, and potential complications of torus removal is essential for providing optimal care. While these bony prominences appear straightforward in presentation, their surgical management requires careful attention to surrounding anatomical structures and meticulous technique to prevent complications like hemorrhage, mucosal sloughing, and perforation into adjacent spaces.
This comprehensive guide examines the clinical characteristics, classification, and surgical management of tori, with special focus on torus palatinus and lingual tori. By understanding the appropriate indications for intervention and mastering the technical aspects of these procedures, dental professionals can confidently incorporate torus removal into their pre-prosthetic treatment protocols.
Table of Contents
- Understanding Tori: Characteristics and Classification
- Indications for Torus Removal
- Torus Palatinus Removal Technique
- Lingual Tori Management
- Instrumentation and Surgical Approach
- Prevention and Management of Complications
- Postoperative Care and Healing
1. Understanding Tori: Characteristics and Classification
1.1 Definition and Etiology
Tori are innocuous bony outgrowths that develop on the oral surfaces of the maxilla and mandible. While their exact etiology remains unclear, several factors may contribute to their development:
- Genetic predisposition appears to play a significant role
- Superficial trauma may trigger development or expansion
- Functional responses to masticatory forces may contribute to growth
- Malocclusion has been associated with tori formation in some patients
Despite considerable research, the precise mechanisms governing tori formation remain incompletely understood, suggesting a multifactorial etiology.
1.2 Classification Systems
Several classification systems exist for characterizing tori based on their size, morphology, and distribution.
For torus palatinus, classification based on size as proposed by Haugen includes:
- Type A: Less than 2 mm in height
- Type B: 2-4 mm in height
- Type C: More than 4 mm in height
This system was later modified by Reichart to include:
- Grade I: Up to 3 mm
- Grade II: Up to 6 mm
- Grade III: Above 6 mm
For lingual tori, Kolas proposed a classification based on number and placement:
- Bilateral single
- Bilateral multiple
- Unilateral single
- Unilateral multiple
These classification systems guide both surgical planning and communication between clinicians.
2. Indications for Torus Removal
2.1 Prosthetic Considerations
The primary indications for torus removal relate to prosthodontic rehabilitation:
- Tori that preclude smooth placement of complete or partial dentures
- Prominences that create pressure points beneath denture bases
- Large tori that interfere with peripheral seal, compromising retention
- Bony protuberances that destabilize the prosthesis during function
For dentate individuals, tori rarely require removal unless they interfere with function or create persistent discomfort.
2.2 Additional Indications
Beyond prosthetic considerations, other indications for torus removal include:
- Recurrent mucosal surface trauma during mastication
- Frequent ulceration of the overlying mucosa
- Deep undercuts and multiple nodules that create food traps
- Psychological concerns expressed by the patient
- Use as donor sources for autogenous bone grafts in selected cases
The decision to remove tori should always balance the benefits against the risks and morbidity associated with the procedure.
3. Torus Palatinus Removal Technique
3.1 Anatomical Considerations
Torus palatinus presents as a benign, slowly growing bony projection of the palatine processes of the maxillae. These growths typically develop bilaterally along the median suture on the oral surface of the hard palate. The overlying mucosa is usually thin and tightly bound to the underlying bone, requiring careful management during surgery.
Key anatomical considerations include:
- Proximity to the greater palatine vessels
- Relationship to the nasal floor
- Thickness of the palatal bone
- Quality and quantity of the overlying mucosa
Understanding these relationships is essential for safe and effective surgical intervention.
3.2 Surgical Procedure
The surgical removal of torus palatinus follows these key steps:

- Access and Exposure: Create a double Y incision (open-door technique) or midline incision. Reflect the flap with a periosteal elevator and secure it to the mucosa of the alveolar process to keep it out of the operative field.
-
Bone Removal: The approach depends on the size and morphology of the torus:
- For small pedunculated tori: Cleave with a sharp chisel and mallet
- For broad-based tori: Cut crisscross grooves with a carbide fissure bur, divide into small segments, and remove pieces with rongeur forceps or mallet and chisel
- Surface Preparation: Use bone files, chisels, or large bone burs to smooth the surface after torus removal. Trim any surplus mucosa with scissors if desired.
- Closure: Close with non-absorbable sutures. Use everted edges with mattress sutures for thicker midline mucosal covering. Prevent hematoma formation with a rubber drain, splint, or stent.
This systematic approach minimizes complications while effectively removing the torus.
4. Lingual Tori Management
4.1 Anatomical Considerations
Lingual tori appear on the lingual aspect of the mandibular alveolar ridge, typically in the canine and premolar regions. Their size and shape vary considerably, with some presenting as pedicled growths and others as broad-based structures.
Critical anatomical considerations include:
- Proximity to the lingual nerve
- Relationship to the submandibular duct
- Location of the sublingual veins
- Attachment of the mylohyoid muscle
These anatomical relationships increase the complexity and potential morbidity of lingual tori removal compared to palatine tori.
4.2 Surgical Procedure
The surgical removal of lingual tori involves the following steps:

- Incision and Exposure: Create an intrasulcular incision without releasing, extending from the lingual midline to beyond the posterior limit of the tori. For edentulous cases, place the incision in the crest of the alveolar ridge.
- Flap Management: Raise a full-thickness flap, taking care to protect the lingual nerve. Small tori can be removed directly with a bur, while larger tori require creation of a cleavage plane with a bur, completed by osteotomes.
- Bone Removal and Contouring: After removing the tori, check the surface for irregularities. Use rongeur forceps and bone files to remove any remaining irregularities.
- Closure: Reposition the flap and secure with appropriate sutures, ensuring tension-free closure.
This procedure requires meticulous technique to avoid damage to vital structures in the floor of the mouth.
5. Instrumentation and Surgical Approach
5.1 Key Instruments
Successful torus removal requires appropriate instrumentation:
- Chisels and osteotomes: Essential for splitting and cleaving tori
- Mallet: Used in conjunction with chisels and osteotomes
- Rotary instruments: Including carbide burs for bone cutting and shaping
- Rongeur forceps: For removing bone fragments
- Bone files: For smoothing irregular surfaces after initial removal
- Periosteal elevators: For atraumatic flap reflection
Proper instrument selection enhances efficiency and reduces surgical trauma.
5.2 Flap Design and Management
Appropriate flap design is critical for access, visibility, and wound healing:
- For torus palatinus, a double Y or midline incision provides optimal access
- For lingual tori, an intrasulcular or crestal incision offers the best approach
- Flaps should be of adequate thickness to maintain vascularity
- Tension-free closure is essential for primary healing
- Proper flap reflection and protection minimize trauma to vital structures
These principles guide successful flap management across all tori removal procedures.
6. Prevention and Management of Complications
6.1 Potential Complications
Despite careful technique, complications can occur following tori removal:
For torus palatinus removal, potential complications include:
- Hemorrhage from greater palatine vessels
- Hematoma formation beneath the flap
- Sloughing of palatal mucosa
- Perforation into the floor of the nose
- Fracture of the palate in severe cases
For lingual tori removal, complications may include:
- Injury to the submandibular salivary gland duct
- Excessive bleeding from floor of mouth vessels
- Laceration of the mylohyoid muscle
- Tearing of the flap during elevation
- Life-threatening hemorrhage in the floor of the mouth
- Infection with potential spread to deep fascial spaces
- Airway obstruction secondary to bleeding or edema
Early recognition and appropriate management minimize the impact of these complications.
6.2 Preventive Strategies
Several strategies help prevent complications during tori removal:
- Thorough preoperative assessment, including radiographic evaluation
- Identification of high-risk patients, particularly those with bleeding disorders
- Meticulous surgical technique with careful tissue handling
- Protection of adjacent anatomical structures during surgery
- Adequate hemostasis before wound closure
- Appropriate postoperative instructions and follow-up
Implementation of these preventive strategies significantly reduces complication risks.
7. Postoperative Care and Healing
7.1 Immediate Postoperative Management
Proper postoperative care enhances healing and patient comfort:
- Pain management with appropriate analgesics
- Antimicrobial therapy when indicated
- Cold compresses to minimize edema
- Dietary modifications during the initial healing phase
- Oral hygiene instructions with emphasis on gentle care around the surgical site
Patient compliance with these recommendations significantly influences healing outcomes.
7.2 Long-Term Follow-Up
Long-term monitoring ensures optimal healing and prosthetic outcomes:
- Evaluation of wound healing at appropriate intervals
- Assessment of ridge contour after complete healing
- Timing of prosthetic rehabilitation based on healing progress
- Addressing any persistent irregularities or soft tissue concerns
- Instructions for prosthesis maintenance and care
This comprehensive follow-up ensures successful transition to the prosthetic phase of treatment.
What are the differences between torus removal, frenectomy, and ridge augmentation in pre-prosthetic surgery?
Torus removal, frenectomy, and ridge augmentation represent distinct pre-prosthetic procedures addressing different anatomical limitations that impact prosthetic success.
Torus removal addresses excess bony structures that interfere with denture placement and adaptation. These procedures are reductive in nature, selectively removing benign bony outgrowths from the palate (torus palatinus) or the lingual aspect of the mandible (lingual tori). The primary goal is to eliminate physical interferences with denture placement, creating a smooth surface for prosthetic adaptation. These procedures are typically performed with chisels, burs, and rongeurs under local anesthesia, with careful attention to the thin overlying mucosa.
Frenectomy, in contrast, focuses on soft tissue attachments that limit denture extension or compromise peripheral seal. This procedure removes or repositions abnormal frenal attachments (labial or lingual) that would otherwise displace the denture during functional movements. The technique employs soft tissue excision with primary closure, often incorporating Z-plasty principles to prevent scar contracture. Unlike torus removal, frenectomy addresses soft tissue limitations rather than bony prominences.
Ridge augmentation fundamentally differs from both procedures in that it is additive rather than reductive, focusing on increasing ridge dimensions in severely resorbed cases. These procedures employ autogenous bone grafts, alloplastic materials, or combinations to increase ridge height and width. The techniques range from onlay grafting to guided bone regeneration, often utilizing membranes and fixation devices. While torus removal and frenectomy typically yield immediate prosthetic benefits, ridge augmentation requires significant healing time before prosthetic rehabilitation can proceed.
The selection among these procedures depends on patient-specific limitations, with comprehensive assessment guiding appropriate intervention choice.
What complications can arise after torus removal procedures, and how are they managed?
Torus removal procedures, while generally safe, can result in several complications requiring prompt recognition and management.
Hemorrhage represents the most common immediate complication, particularly with palatine tori where the greater palatine vessels may be encountered. Management includes direct pressure, hemostatic agents, and in severe cases, vessel ligation or electrocautery. Prevention involves careful surgical planning and identification of vascular structures preoperatively.
Hematoma formation beneath the mucosal flap may compromise healing and increase infection risk. Management includes evacuation, pressure dressings, and in some cases, surgical re-entry for clot removal and hemostasis. Preventive strategies include effective hemostasis before closure and appropriate postoperative pressure application.
Soft tissue necrosis or mucosal sloughing occurs when flaps are designed too thin or with inadequate blood supply. Management involves conservative debridement, antimicrobial therapy, and supportive care until secondary healing occurs. Prevention includes proper flap design with adequate thickness and tension-free closure.
Perforation into adjacent anatomical spaces presents a serious complication, particularly perforation into the nasal floor during palatine tori removal or into the floor of the mouth during lingual tori removal. Management depends on the size of the perforation, ranging from conservative observation to surgical repair. Prevention involves careful depth assessment during bone removal and appropriate instrumentation.
Infection following torus removal typically responds to antimicrobial therapy and local wound care. More severe infections, particularly involving the floor of the mouth, may require incision and drainage along with broader-spectrum antibiotics. Prevention includes aseptic technique and prophylactic antibiotics for high-risk patients.
Early recognition and appropriate management of these complications minimize their impact on healing and prosthetic outcomes. Most complications resolve with conservative measures when identified promptly and managed appropriately.
Conclusion
Torus removal represents an essential component of pre-prosthetic surgery, addressing bony prominences that would otherwise compromise denture fabrication, stability, and patient comfort. Through understanding the classification, indications, and surgical management of both palatine and lingual tori, dental practitioners can effectively incorporate these procedures into comprehensive pre-prosthetic care.
The technical aspects of torus removal require careful attention to surrounding anatomical structures, appropriate instrumentation, and meticulous surgical technique. By following established protocols for flap design, bone removal, and wound closure, clinicians can achieve predictable results while minimizing potential complications.
Patient selection remains critical, with intervention primarily indicated for edentulous patients requiring prosthetic rehabilitation. Through comprehensive preoperative assessment, proper surgical execution, and appropriate postoperative care, torus removal effectively eliminates these anatomical barriers to successful prosthetic outcomes.
For dental students and practitioners involved in prosthodontic rehabilitation, mastery of these techniques provides an essential foundation for addressing the comprehensive needs of edentulous patients. When incorporated into a broader pre-prosthetic approach including alveoloplasty, vestibuloplasty, and ridge augmentation when indicated, torus removal contributes significantly to the establishment of an optimal environment for prosthetic success.