Alveolar Ridge Correction in Pre-Prosthetic Surgery: Methods, Indications, and Exam-Focused Insights
Medi Study Go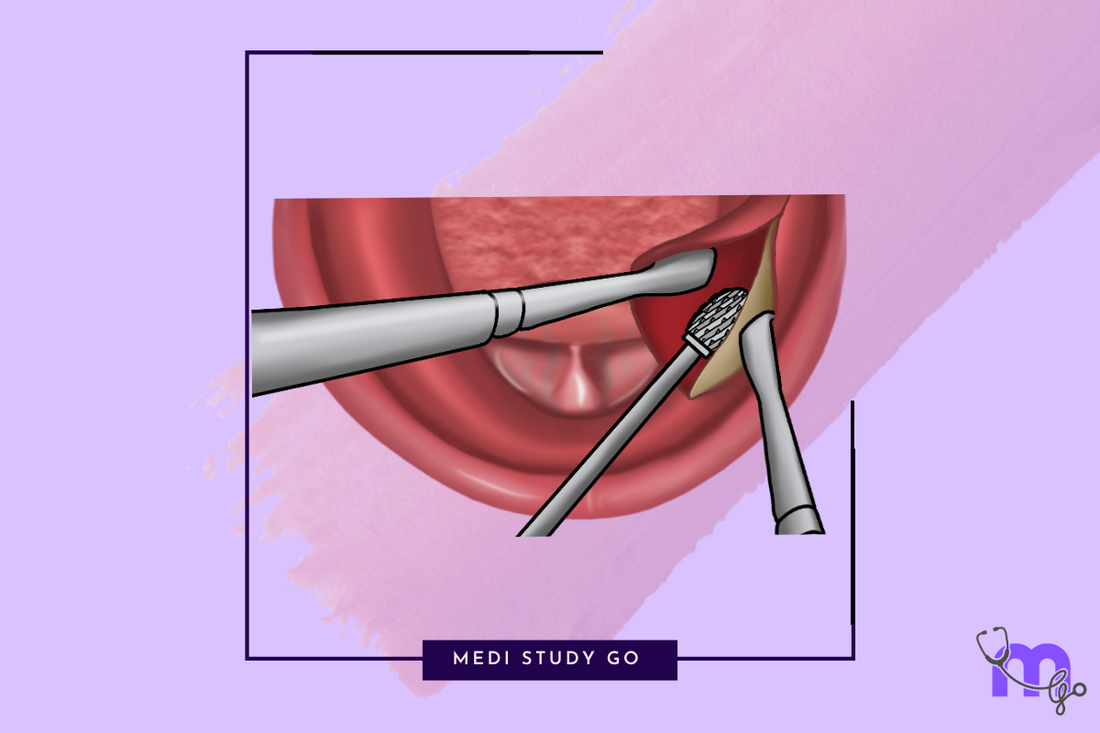
Related Resources:
- Comprehensive Guide to Pre-Prosthetic Surgery: Techniques, Indications, and Clinical Relevance for Dental Students
- Alveoloplasty: Procedure, Clinical Applications, and Key Points
- Vestibuloplasty Techniques: Comparative Review and Clinical Decision-Making
- Torus Removal in Pre-Prosthetic Surgery: Indications, Surgical Steps, and Complications
- Ridge Augmentation and Frenectomy: Modern Approaches and Evidence-Based Outcomes
Key Takeaways:
- Alveolar ridge correction procedures aim to create optimal supporting structures for denture stability
- Techniques include reduction of sharp mylohyoid ridges and genial tubercles, various alveoloplasty methods, and treatment of bony irregularities
- Patient-specific anatomical assessment is critical for selecting appropriate surgical approach
- Proper surgical technique minimizes complications and maximizes denture function
- These procedures significantly improve prosthetic outcomes in patients with challenging ridge anatomy
Introduction
Alveolar ridge correction forms the foundation of successful pre-prosthetic surgery, addressing bony irregularities that would otherwise compromise denture fit, stability, and patient comfort. For dental professionals specializing in prosthodontics and oral surgery, mastering these techniques is essential for achieving optimal functional and esthetic outcomes in edentulous patients.
The alveolar ridge undergoes significant remodeling following tooth extraction, often resulting in irregular contours, sharp edges, and bony prominences that create challenges for denture fabrication and wear. Surgical correction of these irregularities creates a more favorable foundation for prosthetic rehabilitation by establishing appropriate ridge height, width, and morphology.
This comprehensive guide examines the most important alveolar ridge correction procedures in pre-prosthetic surgery, including reduction of the mylohyoid ridge and genial tubercles, various alveoloplasty techniques, and approaches for managing common bony irregularities. With a focus on clinical application and exam-relevant details, this article provides essential knowledge for dental students and practitioners working with edentulous patients.
Table of Contents
- Fundamentals of Alveolar Ridge Anatomy
- Ridge Reduction Procedures
- Alveoloplasty Techniques
- Management of Bony Irregularities
- Clinical Decision-Making and Case Selection
- Preventing and Managing Complications
1. Fundamentals of Alveolar Ridge Anatomy
1.1 Post-Extraction Ridge Dynamics
Understanding the natural progression of alveolar ridge remodeling is essential for planning appropriate corrective interventions. Following tooth extraction, the alveolar ridge undergoes predictable changes:
- Initial blood clot formation and granulation tissue development
- Bone formation within the socket over 4-6 weeks
- Progressive resorption of the buccal plate
- Overall ridge height reduction, more pronounced in the buccolingual dimension
- Development of knife-edge ridges, particularly in the anterior maxilla and mandible
These changes often create anatomical challenges that require surgical correction before successful prosthetic rehabilitation.
1.2 Anatomical Considerations in Ridge Assessment
Comprehensive evaluation of the alveolar ridge should include assessment of:
- Ridge height and width dimensions
- Presence of undercuts and irregular contours
- Relationship of the ridge to adjacent anatomical structures
- Quality and quantity of overlying soft tissue
- Presence of bony prominences (mylohyoid ridge, genial tubercles, tori)
Radiographic assessment using panoramic radiographs and cone-beam computed tomography (CBCT) provides valuable information about internal bone architecture and proximity to vital structures.
2. Ridge Reduction Procedures
2.1 Mylohyoid Ridge Reduction
The mylohyoid ridge is a bony prominence on the lingual aspect of the mandible that can interfere with denture extension and cause chronic irritation of the overlying mucosa. Prominent mylohyoid ridges typically cause:
- Friction on mucosa with denture movement
- Frequent ulceration and pain
- Compromised peripheral seal along the lingual flange
The surgical procedure for mylohyoid ridge reduction follows these steps:

- Create a crestal incision in the posterior ridge region with an oblique releasing incision at the distal end toward the buccal cheek (to avoid lingual nerve damage)
- Reflect a mucoperiosteal flap on the lingual side, using a flat blade of a tongue depressor between flap and bone for protection
- Reduce the mylohyoid ridge using an osteotome or round bur, dissecting mylohyoid muscle fibers away and smoothing with a bone file
- Return and suture the soft tissue flap after complete smoothening
Careful technique avoids damage to the lingual nerve while creating a smooth contour that accommodates denture extension.
2.2 Genial Tubercle Reduction
Genial tubercles are bony projections on the lingual surface of the mandibular symphysis that serve as attachment points for the genioglossus and geniohyoid muscles. When prominent, these tubercles can:
- Create a shelf-like projection that dislodges lower dentures
- Eliminate peripheral seal on the lingual aspect
- Cause frequent ulceration of the overlying mucosa
The procedure for genial tubercle reduction involves:
- Creating a crestal incision from the right to left canine regions
- Reflecting a full-thickness mucoperiosteal flap on the lingual side (without reflection on the labial side)
- Carefully separating muscle attachments with sharp dissection
- Securing the genioglossus muscle with a suture to prevent retraction
- Excising the genial tubercle with a round bur or rongeurs
- Smoothing the bone with a file
- Reattaching the genioglossus muscle at the geniohyoid attachment level
- Closing the flap with sutures
This procedure requires careful management of muscle attachments to prevent tongue retraction and potential airway compromise.
3. Alveoloplasty Techniques

3.1 Simple Alveoloplasty
Simple alveoloplasty is typically performed at the time of tooth extraction to prepare the ridge for prosthetic rehabilitation. This procedure:
- Trims buccal or palatal cortical margins after tooth extraction
- Is particularly useful for overerupted teeth requiring vertical reduction
- Typically uses an envelope or trapezoidal flap for access
- Employs rongeur bone-cutting forceps for bone removal
- Following Schram's principle, removes half the desired amount of bone initially
The technique establishes a smoother contour for denture support while preventing sharp edges that could impede healing or cause future mucosal trauma.
3.2 Dean's Alveoloplasty

Dean's alveoloplasty represents a conventional technique for reshaping the alveolar ridge after multiple extractions. The procedure follows a systematic approach:
- Perform multiple extractions
- Reduce the interdental septal bone
- Create vertical cuts at distal ends
- Join vertical cuts with horizontal cuts at the base of the socket
- Fracture the labial cortex
- Compress the fractured buccal plate and close the wound
This comprehensive technique is particularly valuable for preparing the ridge for immediate denture placement, creating a uniform contour that facilitates stable prosthetic support.
3.3 Obwegeser Modification
For cases of extreme premaxillary protrusion or significant ridge irregularities, the Obwegeser modification offers an enhanced approach:
- Fractures both labial and palatal cortices
- Provides more aggressive recontouring for severe deformities
- Effectively addresses extreme premaxillary protrusion
- Can be used on both posterior and anterior ridges
- Creates ideal foundation for immediate denture placement
This more aggressive modification is reserved for cases where standard alveoloplasty would be insufficient to create an appropriate ridge contour.
4. Management of Bony Irregularities
4.1 Buccal Undercuts
Buccal undercuts represent areas where the buccal cortical plate curves inward beneath the crest of the ridge, creating challenges for denture insertion and removal. Management approaches include:
- Selective alveoloplasty to reduce the prominence of the undercut
- Surgical recontouring using rongeurs and rotary instruments
- In severe cases, segmental ridge procedures
Alternatively, prosthetic solutions such as altered flange design may be employed when surgical correction is contraindicated.
4.2 Alveolar Compression
Alveolar compression represents a simplified ridge modification technique often performed immediately after extraction:
- Compresses outer and inner cortical plates
- Particularly useful for extractions with buccal cortex expansion
- Reduces socket width and eliminates bony undercuts
- Represents one of the easiest and quickest forms of ridge modification
- Suturing is often optional
While simple, this technique must be applied judiciously to avoid excessive ridge reduction or compromise of adjacent structures.
5. Clinical Decision-Making and Case Selection
5.1 Patient Assessment and Evaluation
Appropriate case selection for alveolar ridge correction begins with comprehensive patient assessment:
- Medical history evaluation for factors affecting bone healing
- Assessment of ridge morphology and dimensions
- Evaluation of soft tissue quantity and quality
- Radiographic analysis of internal bone architecture
- Consideration of patient's prosthetic needs and expectations
These factors collectively guide selection of the most appropriate ridge correction procedures.
5.2 Integrating Ridge Correction with Treatment Planning
Ridge correction should be integrated into comprehensive treatment planning with consideration of:
- Timing of extractions and ridge procedures
- Plans for immediate or conventional denture placement
- Potential for future implant placement
- Need for complementary soft tissue procedures
Staged approaches may be necessary for complex cases requiring multiple corrective procedures.
6. Preventing and Managing Complications
6.1 Common Complications
Potential complications of alveolar ridge correction procedures include:
- Excessive bleeding and hematoma formation
- Nerve damage, particularly to the lingual and mental nerves
- Soft tissue dehiscence during healing
- Inadequate ridge correction requiring secondary procedures
- Excessive bone removal compromising prosthetic support
With proper technique and case selection, most of these complications can be avoided or minimized.
6.2 Postoperative Management
Effective postoperative management includes:
- Appropriate analgesic and antimicrobial therapy when indicated
- Careful tissue handling during suture removal
- Staged prosthetic rehabilitation allowing adequate healing
- Regular assessment of healing progress
- Early intervention if complications arise
In most cases, provisional prostheses should be adjusted or relined to prevent pressure on surgical sites during the initial healing phase.
What are the main indications for alveolar ridge correction before complete denture placement?
Alveolar ridge correction becomes necessary when the existing ridge morphology would compromise denture fit, stability, or patient comfort. The main indications include:
- Sharp or irregular ridge contours creating pressure points
- Prominent mylohyoid ridges interfering with lingual flange extension
- Enlarged genial tubercles destabilizing mandibular dentures
- Deep buccal undercuts preventing proper denture insertion or removal
- Knife-edge ridges unable to withstand occlusal forces
- Overdeveloped maxillary tuberosities interfering with posterior extension
- Excessive bone height requiring reduction for appropriate interarch space
By addressing these anatomical limitations surgically, clinicians create a more favorable foundation for denture fabrication, enhancing long-term prosthetic success and patient satisfaction.
How do procedures like reduction of the mylohyoid ridge improve denture retention and stability?
Mylohyoid ridge reduction significantly enhances denture performance through several mechanisms:
- Eliminates interference with lingual flange extension, allowing optimal coverage of the denture-bearing area
- Prevents denture displacement during functional movements by removing bony prominences
- Creates a smooth, rounded contour that facilitates peripheral seal along the lingual border
- Reduces chronic irritation and ulceration that would otherwise lead to patient discomfort and inconsistent denture use
- Allows for proper tissue adaptation around the denture borders, enhancing retention through capillary action
By removing this anatomical barrier to proper denture extension and adaptation, mylohyoid ridge reduction directly contributes to improved denture stability, retention, and patient comfort.
Conclusion
Alveolar ridge correction procedures represent essential interventions in pre-prosthetic surgery, addressing bony irregularities that would otherwise compromise denture success. Through careful patient assessment, proper surgical technique, and appropriate case selection, these procedures create an optimal foundation for prosthetic rehabilitation.
The techniques described in this article—including mylohyoid ridge reduction, genial tubercle management, and various alveoloplasty methods—provide a comprehensive toolkit for addressing common challenges in ridge preparation. By understanding the indications, techniques, and potential complications of these procedures, dental professionals can significantly enhance prosthetic outcomes for their edentulous patients.
As dental implants continue to evolve as a treatment option, these fundamental ridge correction principles remain relevant, often forming the foundation for implant site preparation. Whether preparing the ridge for conventional dentures or implant-supported prostheses, mastery of these techniques is essential for achieving optimal functional and esthetic results in prosthetic dentistry.