Comprehensive Guide to Pre-Prosthetic Surgery: Techniques, Indications, and Clinical Relevance for Dental Students
Medi Study Go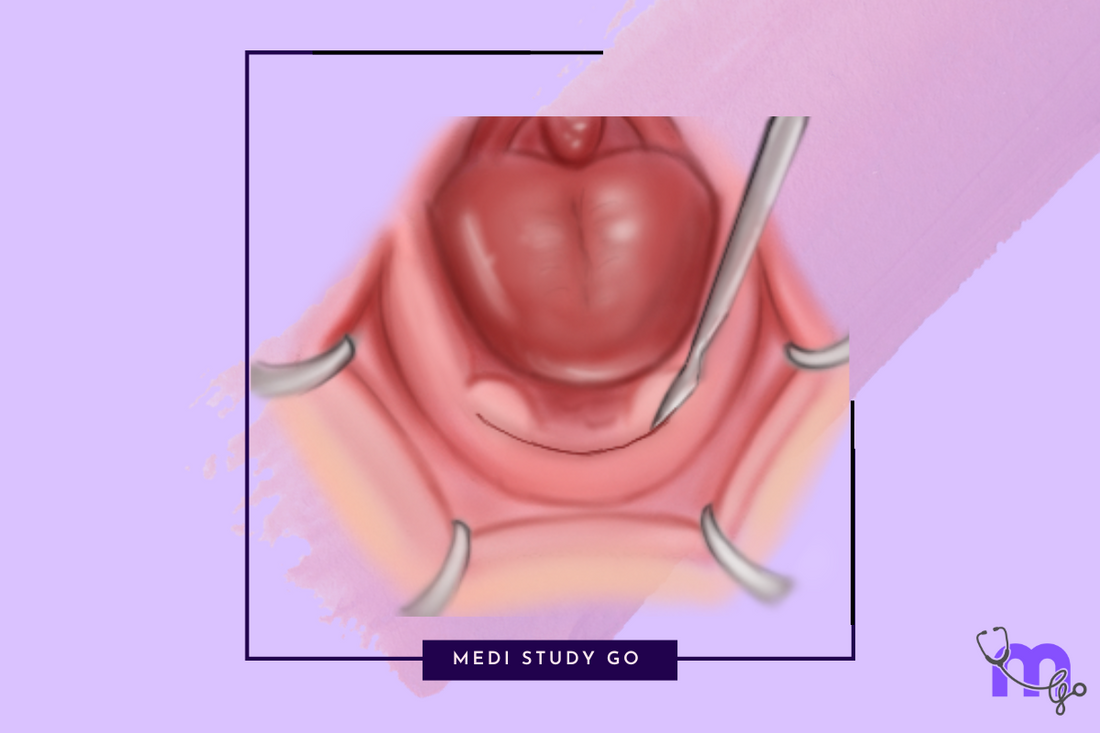
Related Resources:
- Alveolar Ridge Correction in Pre-Prosthetic Surgery: Methods, Indications, and Exam-Focused Insights
- Alveoloplasty: Procedure, Clinical Applications, and Key Points
- Vestibuloplasty Techniques: Comparative Review and Clinical Decision-Making
- Torus Removal in Pre-Prosthetic Surgery: Indications, Surgical Steps, and Complications
- Ridge Augmentation and Frenectomy: Modern Approaches and Evidence-Based Outcomes
Key Takeaways:
- Pre-prosthetic surgery modifies oral tissues to optimize denture fit, stability, and function
- Procedures include alveolar ridge correction, vestibuloplasty, torus removal, and ridge augmentation
- Proper case selection and surgical planning are critical for successful outcomes
- Modern techniques focus on preserving supporting structures while optimizing prosthetic stability
- Thorough clinical evaluation and diagnostic imaging are essential before interventions
Introduction
Pre-prosthetic surgery encompasses a set of specialized surgical interventions designed to prepare the oral environment for the optimal placement and function of dental prostheses. For dental practitioners working with edentulous or partially edentulous patients, understanding these procedures is critical for achieving successful prosthetic outcomes. These surgeries modify the alveolar ridges, surrounding soft tissues, and associated anatomical structures to create an environment that enhances denture stability, retention, and patient comfort.
The primary objective of pre-prosthetic surgery is to establish oral conditions that will support long-term prosthetic success. This includes creating adequate alveolar ridge height and width, ensuring proper vestibular depth, eliminating interfering anatomical structures, and establishing appropriate soft tissue support with keratinized mucosa. By addressing these factors surgically before prosthesis fabrication, clinicians can significantly improve functional outcomes and patient satisfaction.
Modern pre-prosthetic surgery has evolved considerably with advances in surgical techniques, biomaterials, and the increasing integration of dental implants. Today's approaches emphasize preservation of bone and soft tissue while still achieving the structural modifications necessary for prosthetic success. This comprehensive guide examines the most important pre-prosthetic surgical procedures, their indications, techniques, and clinical applications for dental professionals.
Table of Contents
- Fundamentals of Pre-Prosthetic Surgery
- Alveolar Ridge Correction Procedures
- Vestibuloplasty Techniques and Applications
- Management of Exostoses and Tori
- Ridge Augmentation Procedures
- Frenectomy in Pre-Prosthetic Treatment
- Case Selection and Treatment Planning
1. Fundamentals of Pre-Prosthetic Surgery
1.1 Goals and Principles
Pre-prosthetic surgery is fundamentally guided by the need to create optimal conditions for denture support, stability, and function. The primary goals include establishing adequate ridge dimensions, ensuring proper interarch relationships, and creating appropriate soft tissue support. Successful pre-prosthetic surgery aims to:
- Modify denture-bearing areas for stable prosthesis support
- Ensure proper interarch jaw relationships with adequate vertical dimension
- Restore jaw functions including mastication, speech, and swallowing
- Preserve oral structures capable of withstanding masticatory forces
- Provide optimal bony ridge height (minimum 5 mm), width, and contour
- Establish firm, resilient soft tissue support with adequate keratinized mucosa
- Create proper vestibular depth to aid in peripheral seal
These goals are achieved through careful modification of both hard and soft tissues, with a focus on preserving natural structures whenever possible.
1.2 Patient Evaluation and Assessment
Thorough pre-surgical assessment is essential for determining appropriate interventions and predicting outcomes. A comprehensive examination includes:
- Facial esthetic examination
- Detailed intraoral examination
- Evaluation of the alveolar ridge dimensions and contours
- Assessment of supporting soft tissue quality and quantity
- Diagnostic models and radiographic analysis
The evaluation should identify specific anatomical limitations that might compromise prosthetic success, such as inadequate ridge height or width, bony undercuts, muscle attachments, shallow vestibules, or prominent tori and exostoses.
2. Alveolar Ridge Correction Procedures
2.1 Alveoloplasty Techniques
Alveoloplasty represents one of the most common pre-prosthetic procedures, involving recontouring of the alveolar process to create a more favorable foundation for dentures. The procedure may be performed at the time of tooth extraction (simple alveoloplasty) or as a separate surgery (radical alveoloplasty).
Simple alveoloplasty involves trimming and smoothing sharp bony edges and irregular contours after extraction. This procedure:
- Removes sharp bony margins to prevent mucosal trauma
- Reshapes the alveolar ridge to create a more uniform surface
- Helps prevent post-extraction complications
For more extensive ridge irregularities, Dean's alveoloplasty provides a comprehensive approach:
- Multiple extractions are performed
- Interdental septal bone is reduced
- Vertical cuts are made at distal ends
- Vertical cuts are joined with horizontal cuts at the socket base
- The buccal plate is compressed and the wound is closed
The procedure is particularly valuable for preparing the ridge when transitioning to immediate dentures. For cases of extreme protrusion, the Obwegeser modification, which fractures both labial and palatal cortices, may be employed.
2.2 Reduction of Mylohyoid Ridge and Genial Tubercles
The mylohyoid ridge and genial tubercles can create significant challenges for denture stability and comfort when prominent. Surgical reduction is indicated when these structures cause:
- Friction on the overlying mucosa
- Frequent ulceration and pain
- Compromised peripheral seal
For mylohyoid ridge reduction, the procedure typically involves:
- Creating a crestal incision in the posterior ridge region
- Reflecting a mucoperiosteal flap on the lingual side
- Reducing the ridge with an osteotome or round bur
- Smoothing with a bone file and suturing the flap back in position
Genial tubercle reduction follows a similar approach but focuses on the anterior mandible:
- Making a crestal incision from canine to canine
- Reflecting a mucoperiosteal flap on the lingual side
- Careful dissection and management of the genioglossus muscle
- Excision of the tubercle with a round bur or rongeurs
- Closure with appropriate suturing
3. Vestibuloplasty Techniques and Applications
3.1 Principles and Classification
Vestibuloplasty procedures aim to increase the denture-bearing area by extending the depth of the vestibular sulcus. These techniques are particularly valuable when limited vestibular depth compromises denture stability and retention.
The primary purpose of vestibuloplasty is to:
- Extend the vestibular sulcus depth
- Advance neighboring mucosa to line both sides of the sulcus
- Create non-displaceable tissue for improved denture stability
Various techniques are classified based on their approach:
- Submucosal vestibuloplasty
- Secondary epithelization procedures
- Tissue/alloplastic graft vestibuloplasty
3.2 Secondary Epithelization Techniques
Secondary epithelization techniques are among the most commonly employed vestibuloplasty approaches. They include:
Kazanjian Technique: This procedure involves:
- Making an incision in the lip mucosa
- Reflecting a large flap of labial and vestibular mucosa
- Performing supraperiosteal dissection to deepen the sulcus
- Placing the mucosa flap against the periosteum with sutures
- Allowing the donor site to heal by secondary epithelization
Clark's Technique: A modification of Kazanjian's approach:
- Creates an incision on the alveolar ridge rather than the lip
- Employs supraperiosteal dissection to the desired depth
- Positions mucosal flap with mattress sutures
- Leaves the periosteal surface to granulate and epithelialize
For lingual vestibuloplasty, the Trauner technique offers an effective approach, with careful attention to avoiding lingual nerve damage during dissection.
4. Management of Exostoses and Tori
4.1 Torus Palatinus Removal
Torus palatinus presents as a benign bony growth along the midline of the hard palate. While often asymptomatic, these bony prominences can interfere with denture fabrication and function. Removal is indicated when the torus:
- Prevents proper denture adaptation
- Causes mucosal trauma or ulceration
- Creates psychological concerns for the patient
The surgical approach typically involves:
- Creating a double Y or midline incision
- Reflecting a full-thickness mucoperiosteal flap
- Removing the torus with chisels, burs, or rongeurs depending on size
- Smoothing bone edges and careful flap closure
Potential complications include hemorrhage, hematoma, mucosal sloughing, and rarely, perforation of the nasal floor.
4.2 Lingual Tori Management
Lingual tori appear on the lingual aspect of the mandible, typically in the canine and premolar regions. These can vary in size and morphology, with some presenting as pedunculated and others as broad-based structures.
Indications for removal include:
- Large size causing functional impairment
- Recurrent mucosal trauma and ulceration
- Interference with denture seating and stability
The surgical protocol generally involves:
- Creating an intrasulcular or crestal incision
- Raising a full-thickness mucoperiosteal flap
- Removing the tori with burs or osteotomes
- Smoothing the bone surface and suturing the flap
Special attention must be paid to avoid injury to the lingual nerve, submandibular duct, and floor of the mouth structures during this procedure.
5. Ridge Augmentation Procedures
5.1 Indications and Classification
Ridge augmentation becomes necessary when alveolar resorption has progressed to a point where conventional pre-prosthetic procedures cannot establish adequate ridge dimensions. Kent et al. proposed a classification system that guides treatment selection:
- Class 1: Adequate ridge height but inadequate width
- Class 2: Deficient height and width with knife-edge appearance
- Class 3: Ridge resorbed to basal bone with concave form
- Class 4: Resorption of basal bone creating a pencil-thin ridge
The choice of augmentation technique depends on the degree of atrophy, the patient's anatomic limitations, and prosthetic requirements.
5.2 Augmentation Techniques
Several approaches to ridge augmentation exist:
Superior Border Augmentation: Used for insufficient mandibular height or masticatory pain, this technique involves:
- Crestal incision and mucoperiosteal flap reflection
- Placement of rib grafts vertically along the superior border
- Securing the grafts with interosseous wires
- Flap closure for complete graft coverage
Inferior Border Augmentation: This technique, developed by Marx and Sanders and modified by Quinn, adds height to the mandible through:
- Extraoral approach to expose the inferior border
- Placement of shaped rib grafts against the lingual and buccal aspects
- Securing with circumferential wires
- Packing the space with cortical chips
Interpositional Grafting: Indicated when height is adequate but width is insufficient, this technique:
- Uses various materials including autogenous grafts and alloplastics
- Can be combined with osseointegrated implant placement
- Offers improved dimensions for both anterior and posterior regions
6. Frenectomy in Pre-Prosthetic Treatment
6.1 Labial Frenectomy
Hypertrophic or abnormally positioned labial frena can interfere with denture border extension and compromise peripheral seal. Frenectomy is indicated when:
- The frenum causes midline diastema in dentate patients
- Abnormal attachment is irritated by denture flanges
- Periodontal health is compromised
- Speech is impaired
The standard surgical approach involves:
- Elevating and tensing the lip to make the frenum prominent
- Excising the frenum in a diamond-shaped pattern
- Dissecting away from underlying bone with a periosteal elevator
- Removing excess tissue and suturing the wound
Variations include Z-plasty techniques that reorient the tissue fibers to minimize scar contracture.
6.2 Lingual Frenectomy
Ankyloglossia (tongue-tie) can impact denture stability and function in the mandibular arch. Lingual frenectomy is indicated for:
- Restricted tongue movement affecting denture stability
- Functional impairments of speech or swallowing
- Orthodontic or prosthodontic preparation
The procedure typically involves:
- Creating a transverse incision in the frenum midway between the ventral surface of the tongue and sublingual caruncles
- Dissecting and cutting genioglossus muscle fibers if needed
- Closing the wound with interrupted sutures in a different orientation
Special care must be taken to avoid the submandibular ducts and sublingual veins during the procedure.
7. Case Selection and Treatment Planning
7.1 Evidence-Based Decision Making
Successful pre-prosthetic surgery requires thoughtful case selection and comprehensive treatment planning based on:
- Patient-specific anatomical considerations
- Degree of tissue deficiency or excess
- Overall health status and healing capacity
- Prosthetic requirements and expectations
The least invasive procedure that will achieve the desired outcome should always be selected, with careful consideration of risk-benefit ratios.
7.2 Management of Complications
Despite careful planning, complications can occur. Common complications include:
- Bleeding and hematoma formation
- Infection at surgical sites
- Neurosensory disturbances
- Unexpected tissue dehiscence
- Inadequate improvement in ridge dimensions
Prompt recognition and management of these complications are essential for successful outcomes. Postoperative care protocols should be established for each procedure, with clear patient instructions and appropriate follow-up scheduling.
What are the main indications for pre-prosthetic surgery before complete denture placement?
Pre-prosthetic surgery becomes indicated when anatomical limitations would compromise denture success if left unaddressed. The main indications include:
- Inadequate alveolar ridge height or width (less than 5 mm minimum height)
- Sharp or irregular ridge contours causing mucosal trauma
- Prominent muscle attachments that displace the denture
- Insufficient vestibular depth limiting denture extension
- Bony prominences like tori and exostoses interfering with denture placement
- Fibrous or hypertrophic soft tissue requiring recontouring
- Abnormal frenal attachments compromising peripheral seal
When these conditions are present, appropriate surgical intervention before denture fabrication significantly improves long-term prosthetic outcomes and patient satisfaction.
How do procedures like alveoloplasty and vestibuloplasty improve denture retention and stability?
Alveoloplasty and vestibuloplasty fundamentally enhance denture performance by creating more favorable anatomical conditions. Alveoloplasty improves denture retention and stability by:
- Creating a smooth, regular ridge surface for optimal denture adaptation
- Eliminating undercuts that prevent proper denture seating
- Establishing appropriate ridge contours for denture stability
- Reducing pressure points that cause discomfort and sore spots
Vestibuloplasty contributes to denture performance by:
- Increasing the denture-bearing area by extending vestibular depth
- Creating non-displaceable tissue that resists denture displacement
- Improving peripheral seal around denture borders
- Providing adequate space for denture flanges without displacement by muscle attachments
Together, these procedures create a foundation that maximizes denture stability through improved support, retention, and resistance to dislodging forces.
Conclusion
Pre-prosthetic surgery represents a critical interface between oral surgery and prosthodontics, creating the optimal foundation for successful prosthetic rehabilitation. The procedures discussed in this comprehensive guide—including alveolar ridge correction, vestibuloplasty, torus removal, ridge augmentation, and frenectomy—provide essential tools for addressing the anatomical limitations that can compromise denture success.
The modern approach to pre-prosthetic surgery emphasizes tissue preservation while achieving necessary modifications. With careful patient selection, meticulous surgical technique, and proper postoperative care, these procedures significantly enhance prosthodontic outcomes. As dental implants continue to evolve as a treatment option, pre-prosthetic surgical principles remain relevant, often forming the foundation for implant site preparation and optimization.
For dental practitioners working with edentulous and partially edentulous patients, understanding these techniques allows for comprehensive treatment planning and improved patient care. By recognizing when pre-prosthetic surgery is indicated and selecting appropriate interventions, clinicians can significantly enhance prosthetic success and patient satisfaction with removable prostheses.