Alveoloplasty: Procedure, Clinical Applications, and Key Points
Medi Study Go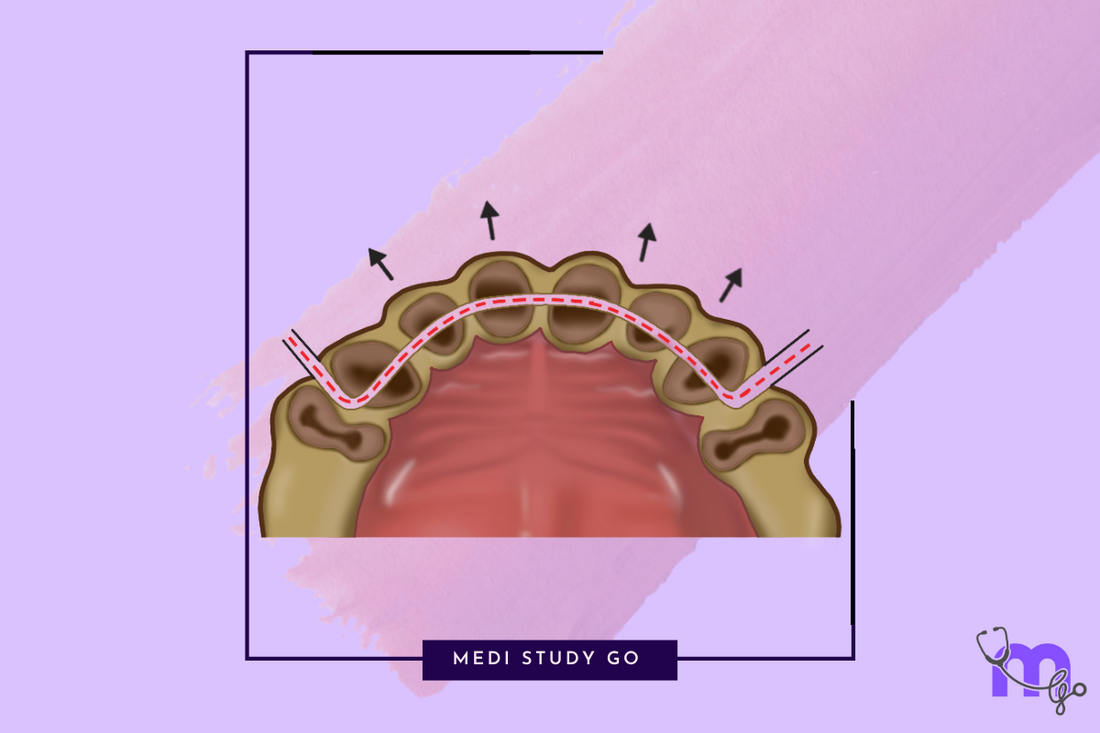
Related Resources:
- Comprehensive Guide to Pre-Prosthetic Surgery: Techniques, Indications, and Clinical Relevance for Dental Students
- Alveolar Ridge Correction in Pre-Prosthetic Surgery: Methods, Indications, and Exam-Focused Insights
- Vestibuloplasty Techniques: Comparative Review and Clinical Decision-Making
- Torus Removal in Pre-Prosthetic Surgery: Indications, Surgical Steps, and Complications
- Ridge Augmentation and Frenectomy: Modern Approaches and Evidence-Based Outcomes
Key Takeaways:
- Alveoloplasty is essential for creating optimal ridge morphology for denture support and stability
- Techniques range from simple alveoloplasty to more complex procedures like Dean's technique
- Proper instrument selection and surgical approach minimize complications
- Effective tissue management and preservation of alveolar bone are crucial for successful outcomes
- Postoperative care significantly influences healing and long-term prosthetic success
Introduction
Alveoloplasty represents one of the fundamental procedures in pre-prosthetic oral surgery, focusing on recontouring the alveolar process to create an optimal foundation for removable prostheses. For dental students and practitioners, mastering the various alveoloplasty techniques is essential for addressing the challenges presented by irregular ridge morphology following tooth extraction or in preparation for prosthetic rehabilitation.
The procedure, which literally means "reshaping the alveolus," encompasses a spectrum of surgical approaches ranging from simple smoothing of sharp edges to comprehensive ridge recontouring. Understanding the principles, techniques, and clinical applications of alveoloplasty enables clinicians to establish the proper foundation for successful prosthetic outcomes, enhancing both function and esthetics for edentulous patients.
This comprehensive guide examines the core concepts of alveoloplasty, including definitions, techniques, instrumentation, and clinical applications. With a focus on practical implementation and evidence-based approaches, this article provides dental students and practitioners with the knowledge necessary to perform these procedures confidently and effectively in clinical practice.
Table of Contents
- Understanding Alveoloplasty: Definitions and Principles
- Classification of Alveoloplasty Techniques
- Simple Alveoloplasty and Alveolar Compression
- Dean's Alveoloplasty Technique
- Instrumentation and Materials
- Clinical Decision-Making and Case Selection
- Postoperative Management and Complications
1. Understanding Alveoloplasty: Definitions and Principles
1.1 Defining Alveoloplasty
In pre-prosthetic surgery, terminology precision is essential for clear communication and procedure planning. Key definitions include:
- Alveolectomy: Excision of a portion of the alveolar process, as described by Boucher
- Alveoloplasty: The recontouring of the alveolar process specifically to prepare the residual ridge for artificial dentures
While these terms are sometimes used interchangeably, alveoloplasty represents the more comprehensive approach to ridge modification, focusing on creating an optimal foundation for prosthetic rehabilitation rather than simply removing bone.
1.2 General Principles of Alveoloplasty
Successful alveoloplasty is guided by several fundamental principles:
- Restructuring or resurfacing alveolar process bone to create a smooth, uniform ridge
- Establishing a functional skeletal relationship between arches
- Preserving as much alveolar bone as possible while eliminating irregularities
- Using simple plasty techniques during extraction to reshape alveolar bone
- Preventing sharp edges that could impede healing or cause future irritation
- Exercising caution against over-compression and excessive bone reduction
These principles underscore the importance of conservative tissue management while achieving the necessary ridge modifications for prosthetic success.
2. Classification of Alveoloplasty Techniques
2.1 Based on Timing
Alveoloplasty procedures can be classified based on their timing relative to tooth extraction:
- Immediate alveoloplasty: Performed simultaneously with tooth extraction
- Secondary alveoloplasty: Conducted as a separate procedure after healing of extraction sites
- Combination alveoloplasty: Includes both immediate modifications and secondary refinements
The timing decision depends on factors including the condition of the alveolar ridge, patient needs, and plans for immediate versus conventional denture delivery.
2.2 Based on Surgical Approach
Alveoloplasty techniques also vary based on the extent and approach to bone modification:
- Simple alveoloplasty: Basic trimming of buccal or palatal cortical margins after extraction
- Alveolar compression: Compression of outer and inner cortical plates
- Dean's alveoloplasty: Conventional technique for comprehensive ridge reshaping
- Obwegeser modification: Advanced technique addressing extreme premaxillary protrusion
The selection of technique depends on the specific ridge morphology, degree of irregularity, and prosthodontic requirements.
3. Simple Alveoloplasty and Alveolar Compression
3.1 Simple Alveoloplasty Technique
Simple alveoloplasty represents the most basic form of ridge modification, typically performed in conjunction with tooth extraction. The procedure includes:
- Trimming buccal or palatal cortical margins immediately after tooth extraction
- Specifically addressing overerupted teeth requiring vertical reduction
- Accessing the surgical site via envelope or trapezoidal flap design
- Removing bone with rongeur bone-cutting forceps
- Following Schram's principle of removing half the desired amount of bone initially
This approach provides immediate ridge smoothing while preserving maximum bone volume.
3.2 Alveolar Compression
Alveolar compression offers a straightforward technique for ridge modification that:
- Represents the easiest and quickest form of ridge reshaping
- Compresses outer and inner cortical plates
- Is particularly suited for extractions with buccal cortex expansion
- Effectively reduces socket width and eliminates bony undercuts
- Often requires no suturing
While simple, this procedure must be performed with care to avoid excessive ridge reduction or compromise of adjacent structures.
4. Dean's Alveoloplasty Technique
4.1 Procedure Steps

Dean's alveoloplasty provides a conventional approach for comprehensive ridge reshaping following multiple extractions. The procedure follows these systematic steps:
- Multiple extractions are performed in the treatment area
- Interdental septal bone is reduced using appropriate instruments
- Vertical cuts are created at the distal ends of the surgical site
- These vertical cuts are joined with horizontal cuts at the base of the socket
- The labial cortex is intentionally fractured along these cut lines
- The fractured buccal plate is compressed and the wound is closed
This technique creates a uniform ridge contour optimal for denture support.
4.2 Obwegeser Modification
For cases of extreme premaxillary protrusion or significant ridge irregularities, the Obwegeser modification enhances the standard approach:
- Fractures both labial and palatal cortices for more comprehensive recontouring
- Specifically addresses extreme premaxillary protrusion cases
- Creates an ideal foundation for immediate denture placement
- Can be applied to both posterior and anterior ridge segments
This modification is typically reserved for cases where standard approaches would be insufficient.
5. Instrumentation and Materials
5.1 Key Instruments for Alveoloplasty
Effective alveoloplasty requires appropriate instrumentation for each phase of the procedure:
- Rotary burs: Used for precise bone contouring, particularly in areas requiring detailed refinement
- Chisels and mallets: Employed for more radical alveoloplasty procedures
- Bone files: Essential for smoothing sharp edges after initial bone removal
- Rongeurs: Used for gross bone removal, particularly in simple alveoloplasty
Proper instrument selection enhances procedural efficiency and outcomes while minimizing trauma to adjacent tissues.
5.2 Surgical Approach and Technique
Beyond instrument selection, surgical technique significantly influences alveoloplasty outcomes:
- Flap design should provide adequate access while ensuring sufficient blood supply
- Bone removal should proceed incrementally, allowing for assessment and adjustment
- Preservation of periosteum enhances healing and minimizes postoperative resorption
- Tension-free flap closure reduces the risk of dehiscence and promotes primary healing
These technical considerations help clinicians achieve optimal results while minimizing complications.
6. Clinical Decision-Making and Case Selection
6.1 Indications for Alveoloplasty
Determining when alveoloplasty is necessary requires careful clinical assessment. Common indications include:
- Significant ridge irregularities following tooth loss
- Sharp bony prominences causing mucosal irritation
- Ridge morphology incompatible with planned prosthetic design
- Excessive ridge height requiring reduction for appropriate interarch relationship
- Bony undercuts interfering with denture insertion or removal
The decision to perform alveoloplasty should balance the benefits of improved ridge morphology against the risks of surgical intervention and potential bone loss.
6.2 Pre-Surgical Assessment
Comprehensive pre-surgical assessment guides procedure selection and planning:
- Clinical examination of ridge morphology and dimensions
- Assessment of soft tissue quality and quantity
- Radiographic evaluation of internal bone architecture
- Consideration of patient's prosthetic needs and expectations
- Evaluation of patient's overall health status and healing capacity
This multifaceted assessment ensures selection of the most appropriate alveoloplasty technique.
7. Postoperative Management and Complications
7.1 Postoperative Care
Effective postoperative management significantly influences healing outcomes:
- Appropriate analgesic therapy to manage postoperative discomfort
- Antimicrobial therapy when indicated based on patient risk factors
- Careful oral hygiene instructions, often including chlorhexidine rinses
- Diet modifications during the initial healing phase
- Clear guidelines for temporary prosthesis use during healing
Patient compliance with these recommendations enhances healing and reduces complication risks.
7.2 Managing Complications
Despite careful technique, complications can occur following alveoloplasty. Common complications include:
- Excessive bleeding or hematoma formation
- Infection at the surgical site
- Dehiscence during healing
- Persistent pain or paresthesia
- Excessive bone removal compromising eventual prosthetic support
Early recognition and appropriate management of these complications minimize their impact on long-term outcomes.
What complications can arise after alveoloplasty procedures, and how are they managed?
Alveoloplasty, while generally safe and effective, can result in several complications that require prompt recognition and management:
Excessive bleeding or hematoma formation typically results from inadequate hemostasis during surgery. Management includes pressure application, use of hemostatic agents, and in severe cases, surgical re-entry for vessel ligation. Preventive measures include thorough preoperative assessment of patients with bleeding disorders and careful surgical technique.
Infection may develop despite aseptic technique, particularly in immunocompromised patients. Management includes drainage if indicated, appropriate antibiotic therapy based on culture sensitivity when possible, and enhanced local wound care. Preventive strategies include perioperative antimicrobial prophylaxis for high-risk patients.
Neurosensory disturbances, particularly involving the lingual or inferior alveolar nerves, can occur during mandibular alveoloplasty. These range from temporary paresthesia to permanent anesthesia. Management is primarily expectant, with microsurgical repair reserved for cases with confirmed nerve transection. Most cases resolve spontaneously within 6-12 months.
Inadequate bone removal or excessive bone reduction represents a technical complication requiring secondary surgical intervention or prosthetic adaptation. Careful preoperative planning and incremental bone removal help prevent these issues.
How should dental students evaluate and plan for alveoloplasty in edentulous patients?
Comprehensive evaluation and planning for alveoloplasty in edentulous patients requires a systematic approach:
Begin with a thorough medical history to identify factors affecting healing potential or increasing surgical risk, including anticoagulant use, immunosuppression, history of radiation therapy, and systemic diseases affecting bone metabolism.
Clinical examination should include assessment of ridge height, width, and contour; identification of bony prominences, undercuts, and irregularities; evaluation of attached keratinized tissue quality and quantity; and assessment of vestibular depth and muscle attachments.
Radiographic analysis provides critical information about internal bone architecture, proximity to vital structures, and the presence of retained roots or pathology. Panoramic radiographs offer a comprehensive overview, while cone-beam computed tomography provides detailed 3D information for complex cases.
Diagnostic casts help visualize the relationship between arches and identify areas requiring modification. Mounting casts in a semi-adjustable articulator aids in assessing interarch space and occlusal relationships.
Integrate findings into a comprehensive treatment plan that considers:
- Type and extent of alveoloplasty needed
- Timing relative to extractions or other procedures
- Plans for immediate or conventional prosthesis delivery
- Need for complementary soft tissue procedures
- Long-term prosthetic goals, including potential for future implant placement
This systematic approach ensures appropriate case selection and technique, maximizing the likelihood of successful prosthetic outcomes.
Conclusion
Alveoloplasty represents a cornerstone of pre-prosthetic surgery, providing essential modification of the alveolar ridge to support successful prosthetic rehabilitation. Through understanding the various techniques, from simple alveoloplasty to more comprehensive approaches like Dean's procedure, clinicians can address the specific challenges presented by each patient's unique ridge morphology.
The key to successful alveoloplasty lies in balancing the need for ridge modification against the importance of preserving alveolar bone. By following the principles of careful tissue management, appropriate instrument selection, and meticulous surgical technique, practitioners can achieve optimal ridge contours while minimizing complications and preserving tissue.
For dental students and practitioners, mastery of alveoloplasty techniques provides an essential foundation for addressing the challenges of prosthetic rehabilitation in edentulous patients. Through careful patient assessment, appropriate procedure selection, and effective postoperative management, alveoloplasty significantly enhances the potential for long-term prosthetic success and patient satisfaction.