Complications of Local Anesthesia: Toxicity, Paresthesia, and Management Protocols
Medi Study Go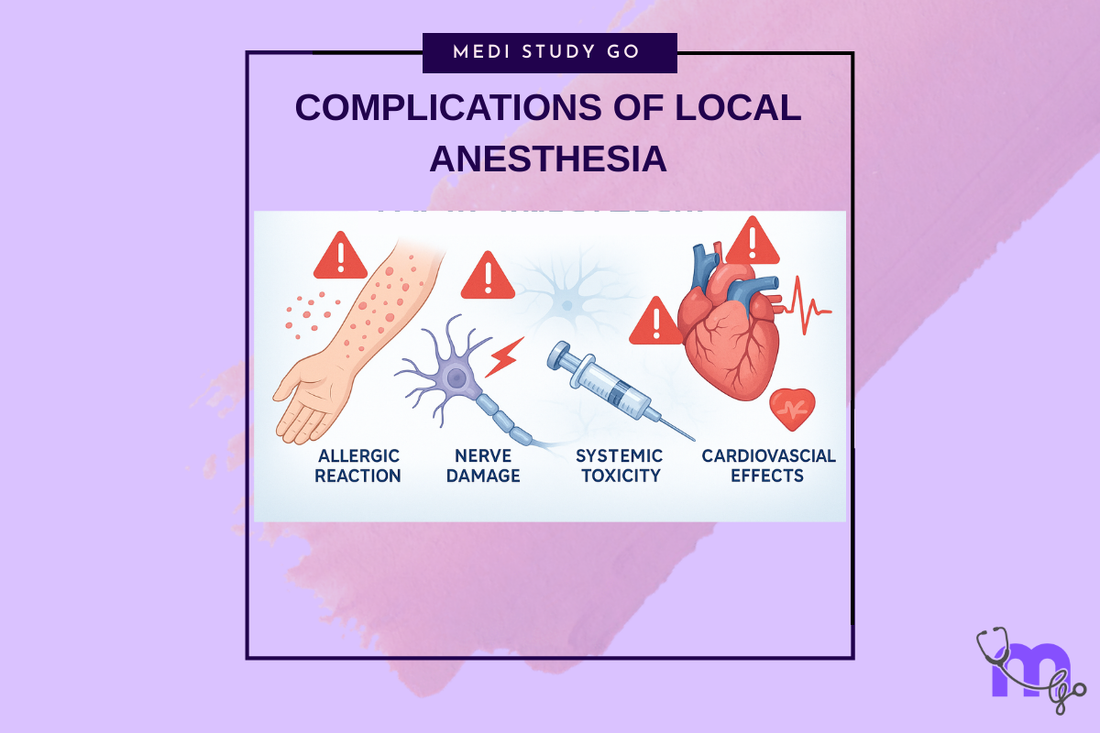
Related Resources
Local and General Anesthesia in Dentistry: Mechanisms, Techniques, and Clinical Applications for Dental Students Theories of Pain and Gate Control Theory: Relevance to Dental Anesthesia Mechanism of Local Anesthetics: Sodium Channel Blockade and Nerve Conduction Classification of Local Anesthetics: Amides vs. Esters and Clinical Selection Criteria Inferior Alveolar Nerve Block: Step-by-Step Technique and Common Errors Dose Calculation and Contraindications for Local Anesthetics in High-Risk Patients Gow-Gates and Closed-Mouth Nerve Blocks: Advanced Techniques for Mandibular Anesthesia Nitrous Oxide in Dentistry: Pharmacology, Sedation Stages, and Safety Protocols Premedication Strategies: Managing Dental Anxiety and Adrenal Insufficiency General Anesthesia in Dental Surgery: Indications, Stages, and Emergency Preparedness Eutectic Mixtures and Topical Anesthetics: Enhancing Patient Comfort in Pediatric Dentistry
Key Takeaways
- Local anesthetic systemic toxicity (LAST) presents with CNS symptoms (tinnitus, seizures) followed by cardiovascular collapse
- Paresthesia following nerve blocks typically resolves within 6-8 weeks, with permanent injury rare but requiring documentation
- Allergic reactions to amide anesthetics are extremely rare (<1%), while ester allergies are more common due to PABA metabolites
- Immediate management of complications requires ABC approach: airway, breathing, circulation, with specific protocols for each complication
- Prevention through proper technique, aspiration, and dose calculation remains superior to treating complications after they occur
While local anesthetics have an excellent safety profile when used correctly, complications can and do occur. Understanding these complications, their prevention, and management protocols is essential for every dental practitioner. This comprehensive guide examines both local and systemic complications, emphasizing recognition, immediate management, and long-term considerations.
Table of Contents
- Systemic Complications and Toxicity
- Local Complications
- Allergic and Idiosyncratic Reactions
- Management Protocols and Emergency Procedures
- Prevention Strategies and Risk Reduction
Systemic Complications and Toxicity
Local Anesthetic Systemic Toxicity (LAST)
LAST represents the most serious complication of local anesthetic administration, resulting from excessive plasma concentrations of the drug. Understanding its pathophysiology, recognition, and management can be life-saving.
Mechanisms of toxicity:
- Direct CNS effects on neurons
- Cardiac sodium channel blockade
- Disruption of cardiac conduction
- Negative inotropic effects
- Vasodilation and hypotension
Risk factors for LAST:
- Inadvertent intravascular injection
- Excessive total dose
- Rapid absorption from vascular areas
- Reduced protein binding states
- Extremes of age (elderly, children)
- Cardiac or hepatic disease
Clinical Presentation of LAST
LAST typically follows a progression from CNS to cardiovascular symptoms:
Early CNS symptoms (excitatory phase):
- Circumoral numbness/tingling
- Metallic taste
- Tinnitus
- Visual disturbances
- Lightheadedness
- Confusion/agitation
Progressive CNS symptoms:
- Muscle twitching
- Tremors
- Seizures (generalized tonic-clonic)
- Loss of consciousness
- Respiratory depression/arrest
Cardiovascular progression:
- Initial hypertension and tachycardia
- Myocardial depression
- Hypotension
- Bradycardia
- Arrhythmias (VT, VF)
- Asystole
Factors Affecting Toxicity
Drug-specific factors:
- Potency (bupivacaine > lidocaine)
- Lipid solubility
- Protein binding
- Rate of systemic absorption
- Presence of vasoconstrictor
Patient factors:
- Body weight
- Metabolic capacity
- Cardiovascular status
- Concurrent medications
- Genetic variations
Overdose Management
Immediate recognition and treatment of LAST is crucial:
Initial management:
- Stop injection immediately
- Call for help
- Maintain airway/give 100% oxygen
- Monitor vital signs
- Establish IV access
Seizure management:
- Benzodiazepines (midazolam 0.05-0.1 mg/kg)
- Avoid phenytoin (cardiac depression)
- Small doses of propofol if needed
- Avoid succinylcholine unless necessary
Cardiovascular support:
- ACLS protocols
- Epinephrine in reduced doses
- Avoid lidocaine, beta-blockers
- Consider vasopressin
- Prepare for prolonged resuscitation
Lipid emulsion therapy:
- 20% lipid emulsion 1.5 mL/kg bolus
- Infusion 0.25 mL/kg/min
- Repeat bolus for cardiovascular instability
- Maximum 10 mL/kg over 30 minutes
Local Complications
Nerve Injury and Paresthesia
Nerve injuries represent one of the most concerning local complications, though permanent damage is rare.
Mechanisms of injury:
- Direct needle trauma
- Intraneural injection
- Chemical neurotoxicity
- Compression from hematoma
- Surgical trauma
Incidence rates:
- Overall: 1:160,000 to 1:785,000
- Higher with certain blocks (IANB)
- Lingual nerve > inferior alveolar nerve
- Most resolve spontaneously
Clinical presentation:
- Immediate onset suggests trauma
- Delayed onset suggests inflammation
- Symptoms: numbness, tingling, pain
- Possible motor dysfunction
- Taste alterations (lingual nerve)
Management approach:
- Document thoroughly
- Reassure patient (most resolve)
- Serial evaluations
- Vitamin B complex (empirical)
- Specialist referral if persistent
- Consider imaging studies
- Avoid re-injection in area
Hematoma Formation
Hematomas result from inadvertent blood vessel puncture:
High-risk injections:
- Posterior superior alveolar (PSA)
- Inferior alveolar nerve block
- Mental/incisive nerve blocks
Clinical signs:
- Rapid swelling
- Discoloration
- Possible trismus
- Patient discomfort
Management:
- Direct pressure (2-3 minutes)
- Ice application
- Patient education
- Monitor for complications
- Antibiotics if indicated
- Document incident
Needle Breakage
Though rare with modern needles, breakage remains a serious complication:
Prevention strategies:
- Never bend needles
- Don't insert to hub
- Use appropriate gauge
- Replace bent needles
- Proper patient management
If breakage occurs:
- Remain calm
- Ask patient not to move
- If visible, attempt retrieval
- Don't probe blindly
- Refer for surgical removal
- Document thoroughly
Trismus
Muscle spasm or fibrosis following injection:
Causes:
- Muscle trauma
- Hematoma formation
- Infection
- Multiple injections
Management:
- Heat therapy
- Gentle stretching exercises
- Muscle relaxants
- Anti-inflammatories
- Physical therapy if persistent
Infection
Post-injection infections are rare but serious:
Risk factors:
- Poor aseptic technique
- Needle contamination
- Immunocompromised patients
- Pre-existing infection
Prevention:
- Sterile technique
- Single-use needles
- Avoid infected areas
- Proper storage
Treatment:
- Appropriate antibiotics
- Drainage if indicated
- Monitor closely
- Document treatment
Allergic and Idiosyncratic Reactions
True Allergic Reactions
Genuine allergic reactions to local anesthetics are rare:
Incidence:
- Amides: <1% of reactions
- Esters: More common (PABA related)
- Often misdiagnosed
Clinical manifestations:
- Urticaria
- Angioedema
- Bronchospasm
- Anaphylaxis
- Delayed reactions
Differential diagnosis:
- Vasovagal reactions
- Anxiety/panic attacks
- Epinephrine effects
- Toxic reactions
Anaphylaxis Management
Life-threatening allergic reaction requiring immediate treatment:
Recognition:
- Rapid onset (minutes)
- Respiratory distress
- Cardiovascular collapse
- Skin manifestations
Treatment protocol:
- Call emergency services
- Epinephrine 0.3-0.5 mg IM
- Oxygen therapy
- Supine position
- IV access/fluids
- Antihistamines
- Corticosteroids
- Prepare for intubation
Idiosyncratic Reactions
Unpredictable responses unrelated to dose:
Methemoglobinemia:
- Associated with prilocaine, benzocaine
- Cyanosis despite normal oxygen
- Methylene blue treatment
- Monitor oxygen saturation
Malignant hyperthermia:
- Extremely rare with locals
- Genetic predisposition
- Rapid temperature rise
- Dantrolene treatment
Management Protocols and Emergency Procedures
Basic Emergency Protocol
All dental offices should have standardized emergency protocols:
Initial assessment (ABC):
- Airway patency
- Breathing adequacy
- Circulation status
- Disability (neurologic)
- Exposure/examination
Emergency equipment:
- Oxygen delivery system
- Automated external defibrillator
- Emergency medications
- Airways/intubation equipment
- IV supplies
Specific Complication Protocols
Syncope/vasovagal reaction:
- Position supine
- Elevate legs
- Oxygen administration
- Monitor vitals
- Aromatic ammonia
- Reassurance
Hyperventilation syndrome:
- Reassurance
- Rebreathing (paper bag)
- Calm environment
- Anxiolytic if needed
Seizures:
- Protect patient
- Oxygen therapy
- Benzodiazepines
- Monitor airway
- Emergency services
Documentation Requirements
Proper documentation protects both patient and provider:
Essential elements:
- Date and time
- Presenting symptoms
- Actions taken
- Patient response
- Consultation/referral
- Follow-up plan
Legal considerations:
- Informed consent
- Standard of care
- Timely referral
- Continuity of care
Prevention Strategies and Risk Reduction
Pre-procedure Assessment
Thorough evaluation prevents many complications:
Medical history review:
- Allergies/reactions
- Current medications
- Medical conditions
- Previous anesthetic experiences
- Pregnancy status
Risk stratification:
- ASA classification
- Specific contraindications
- Alternative techniques
- Consultation needs
Technical Prevention
Proper technique prevents most complications:
Injection technique:
- Proper landmarks
- Appropriate depth
- Aspiration protocol
- Slow injection
- Correct concentration
Dosage considerations:
- Calculate by weight
- Maximum doses
- Cumulative effects
- Vasoconstrictor limits
Patient Communication
Effective communication reduces complications:
Pre-procedure:
- Explain procedure
- Discuss risks
- Address concerns
- Obtain consent
During procedure:
- Continuous monitoring
- Verbal reassurance
- Watch for signs
- Respond promptly
Post-procedure:
- Clear instructions
- Warning signs
- Contact information
- Follow-up plan
Quality Assurance
Continuous improvement enhances safety:
Regular training:
- Emergency protocols
- New techniques
- Complication management
- Team coordination
Equipment maintenance:
- Regular checks
- Proper storage
- Expiration dates
- Emergency supplies
Case review:
- Analyze incidents
- Identify patterns
- Implement changes
- Share learning
Special Populations
Certain patients require extra precautions:
Pediatric patients:
- Weight-based dosing
- Behavioral management
- Parent communication
- Age-appropriate techniques
Elderly patients:
- Reduced doses
- Drug interactions
- Comorbidities
- Slower metabolism
Medically compromised:
- Cardiac patients
- Liver disease
- Bleeding disorders
- Immunosuppression
While complications from local anesthesia are relatively rare, their potential severity demands thorough preparation and immediate recognition. By understanding the mechanisms, maintaining vigilance, and following established protocols, dental professionals can minimize risks and manage complications effectively when they occur. Prevention through proper technique, patient assessment, and continuous education remains the cornerstone of safe local anesthesia practice.
