General Anesthesia in Dental Surgery: Indications, Stages, and Emergency Preparedness
Medi Study Go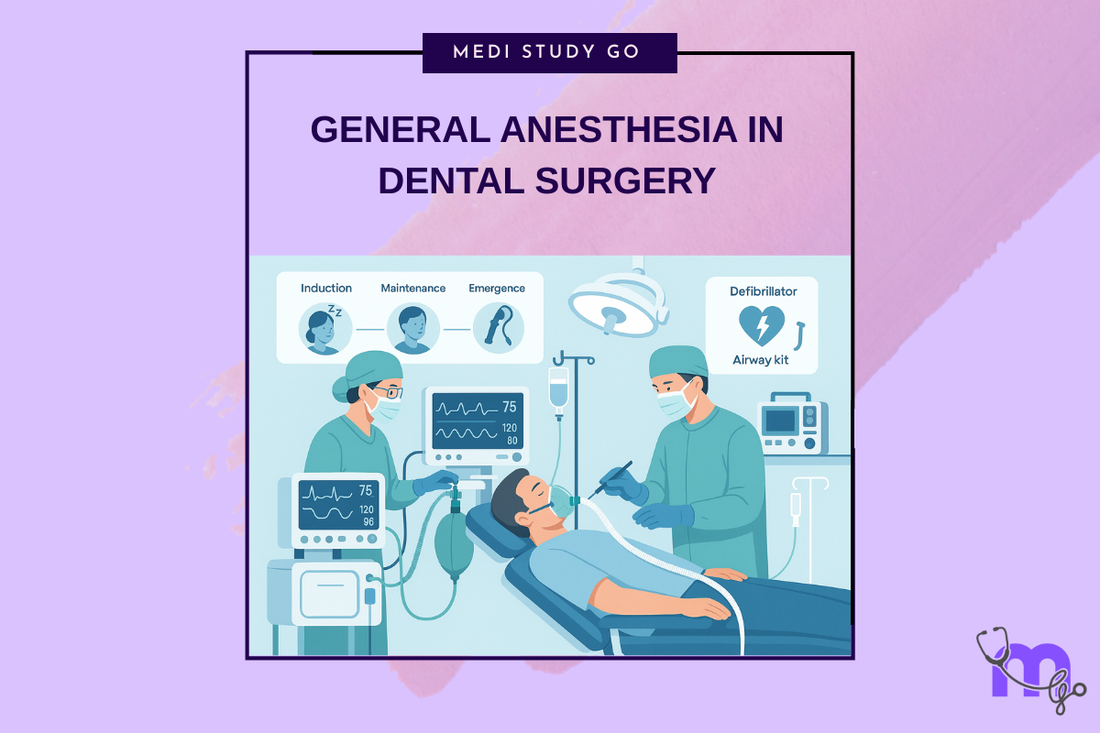
Related Resources
Local and General Anesthesia in Dentistry: Mechanisms, Techniques, and Clinical Applications for Dental Students Theories of Pain and Gate Control Theory: Relevance to Dental Anesthesia Mechanism of Local Anesthetics: Sodium Channel Blockade and Nerve Conduction Classification of Local Anesthetics: Amides vs. Esters and Clinical Selection Criteria Inferior Alveolar Nerve Block: Step-by-Step Technique and Common Errors Complications of Local Anesthesia: Toxicity, Paresthesia, and Management Protocols Dose Calculation and Contraindications for Local Anesthetics in High-Risk Patients Gow-Gates and Closed-Mouth Nerve Blocks: Advanced Techniques for Mandibular Anesthesia Nitrous Oxide in Dentistry: Pharmacology, Sedation Stages, and Safety Protocols Premedication Strategies: Managing Dental Anxiety and Adrenal Insufficiency Eutectic Mixtures and Topical Anesthetics: Enhancing Patient Comfort in Pediatric Dentistry
Key Takeaways
- General anesthesia induces unconsciousness, amnesia, analgesia, and muscle relaxation for complex dental procedures
- The four stages according to Guedel's classification are: analgesia, excitement, surgical anesthesia, and respiratory paralysis
- Proper patient selection, preoperative assessment, and emergency preparedness are crucial for safe administration
- Monitoring includes vital signs, ECG, pulse oximetry, capnography, and anesthetic depth assessment
- Emergency protocols must address airway obstruction, cardiovascular collapse, malignant hyperthermia, and anaphylaxis
General anesthesia represents the most profound level of sedation used in dentistry, reserved for complex surgical procedures and specific patient populations. Understanding its indications, physiological stages, and potential emergencies is essential for dental professionals involved in advanced surgical care. This comprehensive guide examines the principles, practice, and safety considerations of general anesthesia in dental settings.
Table of Contents
- Fundamentals of General Anesthesia
- Indications and Patient Selection
- Stages of General Anesthesia (Guedel's Classification)
- Anesthetic Agents and Techniques
- Emergency Preparedness and Management
Fundamentals of General Anesthesia
Definition and Objectives
General anesthesia is a drug-induced, reversible state characterized by:
Essential components:
- Unconsciousness (loss of awareness)
- Amnesia (no memory formation)
- Analgesia (absence of pain)
- Immobility (muscle relaxation)
- Ablation of autonomic reflexes
Clinical objectives:
- Enable complex surgical procedures
- Ensure patient safety and comfort
- Maintain physiological stability
- Facilitate surgical access
- Prevent psychological trauma
Physiological Impact
General anesthesia affects multiple organ systems:
Central nervous system:
- Cortical depression
- Altered neurotransmission
- Reduced cerebral metabolism
- Modified pain processing
- Suppressed reflexes
Cardiovascular system:
- Myocardial depression
- Vasodilation
- Reduced cardiac output
- Altered baroreceptor function
- Potential arrhythmias
Respiratory system:
- Respiratory depression
- Reduced tidal volume
- Decreased respiratory rate
- Impaired protective reflexes
- Risk of aspiration
Other systems:
- Thermoregulation impairment
- Reduced hepatic blood flow
- Decreased renal perfusion
- Altered endocrine response
- Immune modulation
Types of General Anesthesia
Inhalational anesthesia:
- Delivered via breathing circuit
- Rapid control of depth
- Easy titration
- Common agents: sevoflurane, desflurane, isoflurane
Intravenous anesthesia:
- Direct venous administration
- Rapid onset
- No pollution concerns
- Agents: propofol, etomidate, ketamine
Balanced anesthesia:
- Combination approach
- Multiple drug classes
- Optimized effects
- Reduced side effects
- Standard practice
Indications and Patient Selection
Surgical Indications
Complex procedures requiring general anesthesia:
Maxillofacial surgery:
- Orthognathic procedures
- Facial trauma reconstruction
- Tumor resections
- Extensive bone grafting
- Multiple implant placements
Pediatric procedures:
- Extensive dental rehabilitation
- Multiple extractions
- Behavior management failures
- Special needs patients
- Emergency trauma
Medical indications:
- Severe intellectual disabilities
- Uncontrolled movement disorders
- Extreme dental phobia
- Failed conscious sedation
- Medical conditions precluding cooperation
Patient Assessment
Comprehensive evaluation ensures safety:
Medical history:
- Systemic diseases
- Previous anesthesia experiences
- Current medications
- Allergies and reactions
- Family history (malignant hyperthermia)
Physical examination:
- Airway assessment (Mallampati score)
- Cardiovascular status
- Respiratory function
- Neurological baseline
- Body mass index
Laboratory investigations:
- Complete blood count
- Coagulation studies
- Electrolytes
- Renal function
- Liver function tests
- ECG
- Chest X-ray (if indicated)
Risk Stratification
ASA Physical Status Classification:
ASA I:
- Normal healthy patient
- No systemic disease
- Minimal anesthetic risk
ASA II:
- Mild systemic disease
- No functional limitation
- Examples: controlled hypertension, mild asthma
ASA III:
- Severe systemic disease
- Functional limitation
- Examples: poorly controlled diabetes, COPD
ASA IV:
- Life-threatening disease
- Constant threat to life
- Examples: recent MI, severe heart failure
ASA V:
- Moribund patient
- Survival unlikely without surgery
- Highest risk category
Stages of General Anesthesia (Guedel's Classification)
Stage I: Analgesia/Induction
Initial phase of anesthetic effect:
Characteristics:
- Consciousness maintained initially
- Progressive obtundation
- Analgesia begins
- Reflexes intact
Clinical signs:
- Drowsiness
- Euphoria possible
- Responding to commands
- Normal breathing pattern
Duration:
- Brief with modern agents
- Transition rapid
- Amnesia may begin
Stage II: Excitement/Delirium
Potentially dangerous transition phase:
Characteristics:
- Loss of consciousness
- Uninhibited responses
- Reflex hyperactivity
- Risk of complications
Clinical signs:
- Irregular breathing
- Increased muscle tone
- Dilated pupils
- Possible vomiting
- Uncontrolled movement
Management:
- Rapid progression through stage
- Maintain airway protection
- Avoid stimulation
- Continue anesthetic delivery
Stage III: Surgical Anesthesia
Target depth for procedures:
Plane 1:
- Regular breathing
- Constricted pupils
- Loss of eyelid reflex
- Adequate for minor surgery
Plane 2:
- Fixed pupils
- Loss of corneal reflex
- Intercostal paralysis begins
- Suitable for most surgeries
Plane 3:
- Complete intercostal paralysis
- Dilated pupils
- Diaphragmatic breathing only
- Deep anesthesia level
Plane 4:
- Irregular respiration
- Paradoxical breathing
- Maximum muscle relaxation
- Dangerously deep
Stage IV: Respiratory Paralysis/Overdose
Life-threatening emergency state:
Characteristics:
- Complete respiratory arrest
- Cardiovascular collapse imminent
- Dilated, fixed pupils
- Absent reflexes
Management:
- Immediate intervention
- 100% oxygen
- Respiratory support
- Reduce anesthetic depth
- Cardiovascular support
Anesthetic Agents and Techniques
Induction Agents
Propofol:
- Rapid onset (30-40 seconds)
- Smooth induction
- Antiemetic properties
- Cardiovascular depression
- Pain on injection
Etomidate:
- Hemodynamic stability
- Rapid onset
- Adrenocortical suppression
- Myoclonus common
- Limited by side effects
Ketamine:
- Dissociative anesthesia
- Preserved airway reflexes
- Bronchodilation
- Increased secretions
- Emergence phenomena
Thiopental:
- Barbiturate
- Historical significance
- Rapid onset
- Cardiovascular depression
- Largely replaced
Maintenance Agents
Volatile anesthetics:
Sevoflurane:
- Low blood solubility
- Rapid onset/offset
- Non-irritating
- Suitable for induction
- Minimal metabolism
Desflurane:
- Lowest solubility
- Fastest recovery
- Airway irritation
- Requires vaporizer
- Environmental concerns
Isoflurane:
- Cost-effective
- Stable cardiac output
- Cerebral vasodilation
- Pungent odor
- Still widely used
Intravenous agents:
Propofol infusion:
- Total intravenous anesthesia (TIVA)
- No pollution
- Rapid recovery
- Requires pumps
- Risk of propofol infusion syndrome
Adjuvant Medications
Muscle relaxants:
- Depolarizing (succinylcholine)
- Non-depolarizing (rocuronium, vecuronium)
- Facilitate intubation
- Improve surgical conditions
- Require reversal
Opioids:
- Fentanyl
- Remifentanil
- Morphine
- Provide analgesia
- Reduce anesthetic requirements
Airway Management
Techniques:
- Face mask ventilation
- Laryngeal mask airway (LMA)
- Endotracheal intubation
- Video laryngoscopy
- Fiberoptic intubation
Considerations:
- Patient positioning
- Difficult airway prediction
- Backup plans
- Equipment availability
- Team communication
Emergency Preparedness and Management
Common Emergencies
Airway obstruction:
- Recognition signs
- Head tilt/chin lift
- Jaw thrust
- Oral/nasal airways
- Emergency cricothyrotomy
Laryngospasm:
- Complete airway closure
- Positive pressure ventilation
- Deepening anesthesia
- Succinylcholine if severe
- Prevention strategies
Bronchospasm:
- Wheezing
- Increased airway pressure
- Deepen anesthesia
- Bronchodilators
- Corticosteroids
Cardiovascular Emergencies
Hypotension:
- Common occurrence
- Fluid administration
- Vasopressor support
- Reduce anesthetic depth
- Position changes
Arrhythmias:
- ECG monitoring essential
- Identify cause
- Specific treatments
- ACLS protocols
- Defibrillation ready
Cardiac arrest:
- Immediate CPR
- ACLS algorithms
- Team coordination
- Post-resuscitation care
- Documentation
Rare but Serious Complications
Malignant hyperthermia:
- Genetic predisposition
- Triggered by volatiles/succinylcholine
- Rapid temperature rise
- Muscle rigidity
- Dantrolene treatment
Anaphylaxis:
- IgE-mediated reaction
- Cardiovascular collapse
- Bronchospasm
- Epinephrine treatment
- Supportive care
Awareness under anesthesia:
- Rare but traumatic
- Risk factors known
- Monitoring techniques
- Prevention strategies
- Psychological support
Emergency Equipment
Essential items:
- Advanced airway equipment
- Emergency medications
- Defibrillator
- Suction apparatus
- Oxygen delivery systems
Medications:
- Epinephrine
- Atropine
- Vasopressors
- Bronchodilators
- Dantrolene
- Reversal agents
Team Preparedness
Training requirements:
- ACLS certification
- Regular simulations
- Role assignments
- Communication protocols
- Equipment familiarity
Quality assurance:
- Incident reporting
- Case reviews
- Protocol updates
- Continuing education
- Equipment maintenance
Recovery and Postoperative Care
Emergence criteria:
- Return of consciousness
- Protective reflexes present
- Adequate ventilation
- Stable vital signs
- Pain control
Monitoring requirements:
- Continuous observation
- Vital sign assessment
- Oxygen saturation
- Pain evaluation
- Nausea prevention
Discharge criteria:
- Fully awake
- Stable vital signs
- Ambulatory
- Minimal pain
- No active bleeding
- Responsible escort
General anesthesia in dental surgery requires comprehensive knowledge, meticulous planning, and constant vigilance. Success depends on proper patient selection, understanding anesthetic stages, mastering techniques, and maintaining emergency preparedness. While complications are rare, the ability to recognize and manage them promptly can be life-saving. Continuous education and team training ensure the highest standards of patient safety in dental anesthesia practice.