The Comprehensive Guide to Implant and Maxillofacial Prosthodontics
Medi Study Go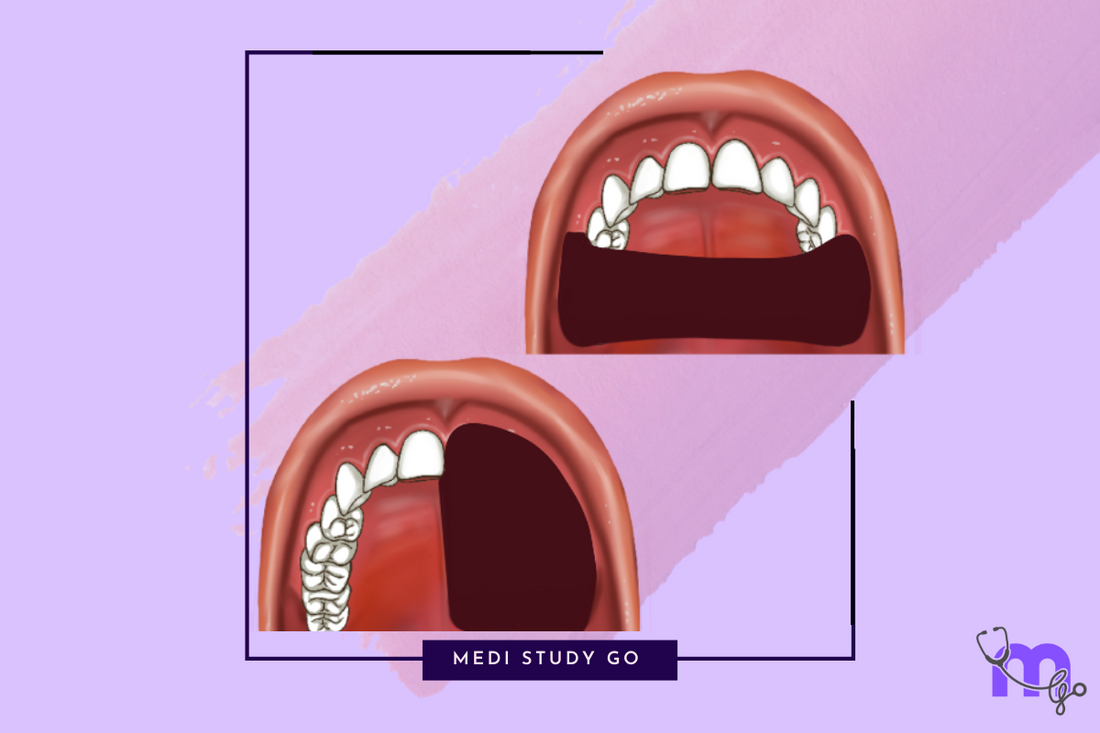
Related Resources
- Understanding Maxillofacial Prosthodontics: Definition and Scope
- Maxillofacial Prosthodontics and Implantology: The Synergistic Relationship
- Implant Placement and Positioning: Where Does the Implant Go?
- Implant Retention and Stability: Effectiveness Without Pulling Out
- Advanced Techniques in Maxillofacial Prosthodontics
Introduction
In the evolving landscape of dental and medical rehabilitation, implant and maxillofacial prosthodontics has emerged as a cornerstone for restoring function, aesthetics, and quality of life for patients with facial defects, missing oral structures, or complex dental needs. This comprehensive guide serves as your gateway to understanding this specialized field, whether you're a dental student preparing for your NEET MDS examination, a practicing professional seeking to expand your knowledge, or an educator guiding the next generation of specialists.
The integration of implant technology with maxillofacial prosthodontics has revolutionized treatment outcomes, providing unprecedented stability, function, and aesthetic results for even the most challenging cases. As advancements in digital technology, biomaterials, and surgical techniques continue to evolve, staying current with best practices in this field has never been more important.
"Maxillofacial prosthodontics represents the intersection of art and science, where surgical precision meets aesthetic creativity to restore not just function, but human dignity."
Throughout this guide, we'll explore the fundamental concepts, latest techniques, and clinical applications that make implant and maxillofacial prosthodontics a vital specialty in modern healthcare. From understanding basic definitions to exploring advanced CAD/CAM technologies, this resource aims to provide a solid foundation for anyone interested in this fascinating field.
What is Maxillofacial Prosthodontics?
Maxillofacial prosthodontics (also known as maxillofacial prosthetics) is a specialized branch of prosthodontics focused on the rehabilitation of patients with defects or disabilities of the head and neck region. These defects may be congenital, developmental, or acquired due to disease, trauma, or surgical treatment.
Definition
According to the American College of Prosthodontists, maxillofacial prosthodontics is defined as:
"The branch of prosthodontics concerned with the restoration and/or replacement of the stomatognathic and craniofacial structures with prostheses that may or may not be removed on a regular or elective basis."
This definition encompasses a wide range of prosthetic interventions, from intraoral devices like obturators for palatal defects to extraoral prostheses such as auricular (ear), nasal, or orbital replacements. The goal is always to restore both function and aesthetics, helping patients reintegrate into society with improved quality of life.
Scope of Practice
Maxillofacial prosthodontists work with a diverse range of patients, including those with:
- Oral cancer and resulting surgical defects
- Congenital defects such as cleft palate
- Traumatic injuries to the face and jaw
- Radiation-induced damage to oral structures
- Neurological conditions affecting oral function
- Developmental anomalies of the maxillofacial region
The scope of this specialty requires collaboration with multiple healthcare professionals, including oral surgeons, oncologists, speech pathologists, and psychological counselors, creating a truly interdisciplinary approach to patient care.
The Relationship Between Implantology and Maxillofacial Prosthodontics
The integration of dental implants with maxillofacial prosthodontics has transformed the field, creating new possibilities for rehabilitation that were previously unattainable. This synergistic relationship has particularly benefited patients with complex maxillofacial defects, offering improved stability, function, and aesthetics for their prostheses.
How Implants Enhance Maxillofacial Prosthetics
Dental implants provide several critical advantages in maxillofacial rehabilitation:
- Enhanced Retention - Implants significantly improve the retention of both intraoral and extraoral prostheses, preventing embarrassing dislodgement during daily activities.
- Preservation of Bone - Unlike conventional prostheses that may accelerate bone resorption, implants help maintain bone volume and density through functional loading.
- Improved Function - Implant-retained prostheses allow for greater bite force and improved chewing efficiency, enhancing nutritional intake and overall health.
- Superior Aesthetics - By eliminating visible clasps and providing better support for prosthetic structures, implants contribute to more natural-looking results.
- Psychological Benefits - The security and confidence provided by implant-retained prostheses can significantly improve patients' psychological well-being and social integration.
The implant-prosthetic connection has become particularly valuable in cases of extensive maxillary resection, where conventional retention methods may be inadequate due to limited remaining structures for support.
Key Topics in Implant and Maxillofacial Prosthodontics
For students preparing for NEET MDS examinations or dental professionals seeking comprehensive knowledge, understanding several core topics is essential for mastering this complex field.

Classification Systems
Several classification systems are used to categorize maxillofacial defects, guiding treatment planning and communication among specialists:
- Aramany's Classification - Categorizes maxillary defects into six classes based on the location and extent of the defect
- Veau's Classification - Focuses on cleft palate defects
- Cantor & Curtis Classification - Addresses mandibular defects
- Kernahan's Striped Y Classification - Used for comprehensive documentation of cleft lip and palate
Types of Maxillofacial Prostheses
Different types of prostheses serve specific rehabilitative needs:
- Obturators - For closing palatal defects, restoring speech and preventing nasal regurgitation
- Facial Prostheses - Including auricular (ear), nasal, orbital, and composite facial prostheses
- Mandibular Resection Prostheses - For rehabilitation after partial mandibulectomy
- Palatal Lift Prostheses - To address velopharyngeal insufficiency
- Speech Aid Prostheses - For improving phonation and articulation
Materials in Maxillofacial Prosthodontics
The selection of appropriate materials is crucial for successful outcomes:
- Silicone Elastomers - Most commonly used for facial prostheses due to their flexibility and lifelike appearance
- Acrylic Resins - Used for intraoral prostheses and prosthesis substructures
- Titanium - The standard material for dental implants due to excellent biocompatibility
- Polyvinyl Siloxane - Preferred impression material for capturing facial defects
Implant Placement and Positioning
A fundamental consideration in implant-supported maxillofacial rehabilitation is determining where the implant goes. Proper implant positioning is critical for both functional outcomes and prosthetic success.
Anatomical Considerations
Several anatomical factors guide implant placement decisions:
- Bone Quality and Quantity - Sufficient bone volume is necessary for implant stability, with special consideration for compromised sites after ablative surgery or radiation
- Critical Structures - Avoiding damage to nerves, blood vessels, sinuses, and adjacent teeth
- Prosthetic Requirements - Positioning that facilitates optimal prosthetic design and function
Advanced Planning Techniques
Modern implant placement relies heavily on digital planning:
- Cone Beam Computed Tomography (CBCT) - Provides 3D visualization of anatomical structures
- Virtual Implant Planning Software - Allows precise positioning and angulation planning
- Surgical Guides - Created through CAD/CAM technology for accurate transfer of the digital plan to the surgical site
Special Considerations in Maxillofacial Cases
Patients requiring maxillofacial rehabilitation often present unique challenges:
- Compromised Bone Sites - Due to previous surgery, trauma, or radiation
- Soft Tissue Considerations - Managing scarred or grafted tissues around implants
- Access Limitations - Overcoming restricted mouth opening or anatomical barriers
Implant Stability and Retention
The long-term success of implant-supported maxillofacial prostheses depends significantly on implant stability and proper retention mechanisms. Understanding how effective the implant is without pulling out requires knowledge of several key factors.
Primary vs. Secondary Stability
Implant stability occurs in two phases:
- Primary Stability - The initial mechanical engagement achieved at implant placement, primarily determined by bone density, implant design, and surgical technique
- Secondary Stability - The biological stability achieved through osseointegration, where bone cells grow directly onto the implant surface
Factors Affecting Implant Stability
Several variables influence whether an implant will remain stable:
- Bone Density - Higher density bone (Type I and II) generally provides better initial stability
- Implant Design - Thread design, diameter, length, and surface characteristics
- Surgical Technique - Proper preparation of the implant site without overheating
- Loading Protocols - Appropriate timing and magnitude of functional loading
- Patient Factors - Systemic health conditions, smoking, and radiation history
Assessment Methods
Clinicians use various techniques to evaluate implant stability:
- Resonance Frequency Analysis - Using devices like Osstell to measure implant stability quotient (ISQ)
- Percussion Testing - Evaluating the sound produced when an implant is tapped
- Torque Testing - Measuring the reverse torque value that an implant can withstand
- Radiographic Evaluation - Assessing bone-implant contact and peri-implant bone levels
Retention Mechanisms for Prostheses
Once stable implants are achieved, various retention systems can secure the prosthesis:
- Bar-Clip Systems - Providing excellent retention for removable prostheses
- Ball Attachments - Offering good retention with simpler design and maintenance
- Magnets - Useful in cases with limited interarch space or for patients with dexterity issues
- Telescopic Systems - Providing rigid support with good aesthetic outcomes
- Screw-Retained Options - For fixed prostheses requiring maximum stability
Advanced Techniques in Maxillofacial Prosthodontics
The field of maxillofacial prosthodontics continues to evolve, with technological advancements creating new possibilities for improved outcomes and more efficient workflows.
Digital Workflow and CAD/CAM Technology
Digital approaches have revolutionized the fabrication of maxillofacial prostheses:
- 3D Facial Scanning - Capturing accurate digital representations of facial anatomy
- Virtual Planning - Designing prostheses with precise contours and dimensions
- Rapid Prototyping - Creating physical models and molds through additive manufacturing
- Direct Fabrication - Producing final prostheses using 3D printing or milling technologies
Impression Techniques
Various impression approaches are used depending on the clinical situation:
- Direct Impression Technique (Open Tray) - Impression copings remain in the impression
- Indirect Impression Technique (Closed Tray) - Impression copings are removed and reattached to the impression
- Digital Impression Systems - Intraoral scanners and facial scanning technology
Emerging Innovations
Several cutting-edge developments are shaping the future of the field:
- Tissue Engineering - Potential for growing replacement tissues rather than fabricating prostheses
- Robotic Surgery - Improving precision in implant placement and reconstructive procedures
- Bioactive Materials - Enhancing the integration between living tissue and prosthetic materials
- Virtual Reality Applications - For patient education and treatment planning
Resources for Dental Students and Professionals
For those preparing for NEET MDS examinations or seeking to expand their knowledge, several resources are invaluable:
Recommended Textbooks
- "Maxillofacial Rehabilitation: Prosthodontic and Surgical Management" by John Beumer III
- "Osseointegration in Craniofacial Reconstruction" by P.D. Worthington and P.I. Brånemark
- "Dental Implant Prosthetics" by Carl E. Misch
Educational Tools
- Flashcard applications for NEET preparation focusing on prosthodontics topics
- NEET previous year question papers with special attention to implant and maxillofacial prosthodontics sections
- NEET mock tests to assess knowledge and exam readiness
- NEET revision tools for last-minute review of key concepts
Professional Organizations
- American Academy of Maxillofacial Prosthetics
- International Society for Maxillofacial Rehabilitation
- Academy of Osseointegration
Conclusion
The field of implant and maxillofacial prosthodontics represents a fascinating intersection of art, science, and compassionate healthcare. For patients with maxillofacial defects, the expertise of professionals in this specialty can truly transform lives, restoring not just function and aesthetics, but also dignity and social confidence.
For dental students preparing for NEET MDS examinations, understanding the fundamentals outlined in this guide provides a solid foundation for success. For practicing professionals, the ongoing advancements in this field offer exciting possibilities to enhance patient care through innovation and evidence-based approaches.
As we continue to witness technological evolution and interdisciplinary collaboration, the future of maxillofacial prosthodontics holds tremendous promise for even more remarkable rehabilitative outcomes.