Implant Placement and Positioning: Where Does the Implant Go?
Medi Study Go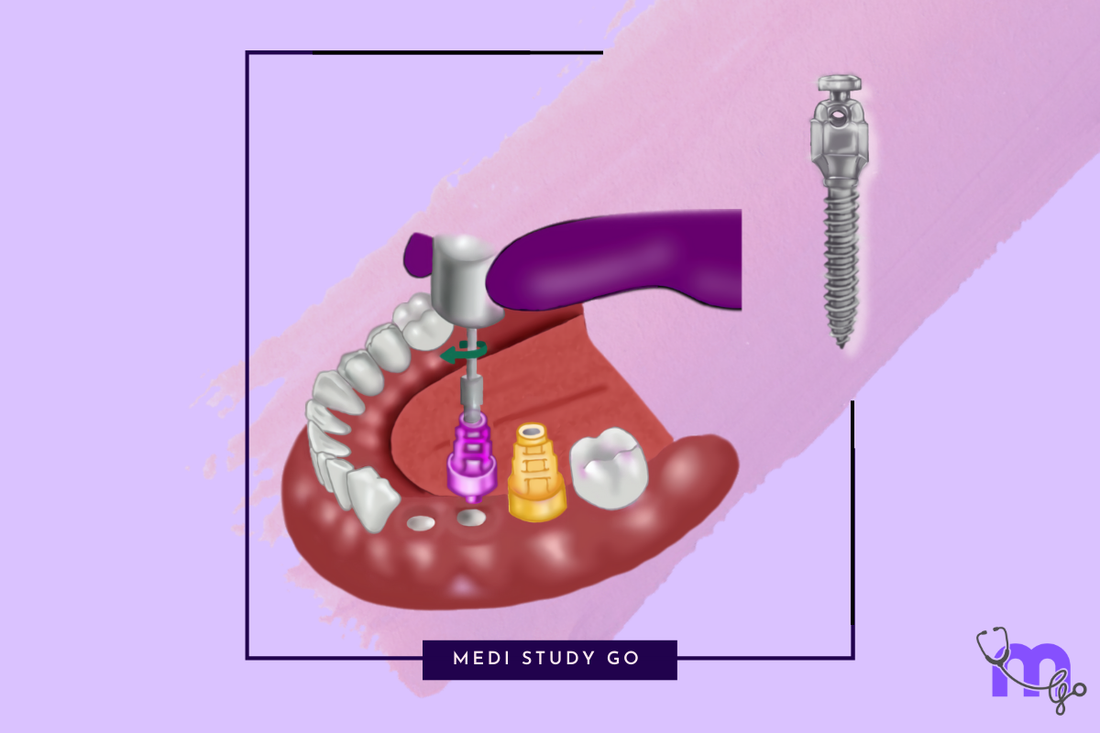
Related Resources:
- Understanding Maxillofacial Prosthodontics: Definition and Scope
- Maxillofacial Prosthodontics and Implantology: The Synergistic Relationship
- Implant Retention and Stability: Effectiveness Without Pulling Out
- Advanced Techniques in Maxillofacial Prosthodontics
Introduction: The Critical Foundation of Successful Implant Therapy
The question of where does the implant go represents perhaps the most fundamental consideration in implant-supported maxillofacial rehabilitation. Proper implant positioning serves as the critical foundation upon which all subsequent prosthetic success depends. When dealing with maxillofacial defects, this question becomes even more complex, as anatomical landmarks may be altered, bone quality compromised, and functional demands increased.
For students preparing for NEET MDS examinations, understanding the principles of strategic implant placement in both standard and compromised situations is essential for mastering advanced concepts in oral rehabilitation. For practicing clinicians, these principles guide critical decisions that will impact patient outcomes for years to come.
"The success of implant therapy is determined long before the implant is even placed - it begins with thorough assessment, precise planning, and a clear vision of the prosthetic outcome."
This article explores the critical factors that determine optimal implant positioning in maxillofacial prosthodontics, from basic anatomical considerations to advanced digital planning techniques.

Foundational Principles: The Prosthetically-Driven Approach
Prosthetic-First Planning Philosophy
The core principle guiding implant placement is that prosthetic requirements should dictate surgical decisions:
- Backward Planning: Beginning with the end in mind - visualizing the final prosthesis
- Restoration-Driven Positioning: Placing implants where they best support the intended prosthesis
- Emergence Profile Consideration: Positioning to create natural contours and transitions
- Biomechanical Optimization: Distributing forces appropriately across the implant-prosthetic complex
The Triad of Optimal Positioning
Ideal implant placement must balance three critical dimensions:
- Mesiodistal Position: Proper spacing between implants and from natural teeth
- Buccolingual Position: Appropriate positioning within the alveolar housing
- Apicocoronal Position: Optimal depth relative to the planned restoration
Each dimension has specific guidelines that must be adapted to individual patient situations.
Anatomical Considerations for Implant Placement
Standard Anatomical Guidelines
Even in non-defect cases, several anatomical structures must be respected:
-
Maxillary Structures:
- Maxillary sinus floor
- Nasopalatine canal
- Incisive foramen
- Adjacent tooth roots
-
Mandibular Structures:
- Inferior alveolar nerve canal
- Mental foramen
- Lingual concavity
- Submandibular gland fossa
Special Considerations in Maxillofacial Defects
Defect cases present additional anatomical challenges:
- Post-Surgical Anatomy: Altered landmarks following resective surgery
- Reconstructed Sites: Variable bone quality in grafted or reconstructed areas
- Irradiated Tissues: Compromised vascularity and healing capacity
- Soft Tissue Alterations: Changes in vestibular depth, attached gingiva, and mucosal quality
- Adjacent Prosthetic Structures: Relationship to obturators or other prosthetic components
Biomechanical Factors in Implant Positioning
The long-term success of implants depends heavily on how forces are distributed through the system.
Force Distribution Principles
Several biomechanical concepts guide optimal positioning:
- Axial Loading: Positioning implants to receive primarily axial rather than off-axis forces
- Crown-to-Implant Ratio: Minimizing unfavorable leverage by maintaining appropriate proportions
- A-P Spread: In full-arch cases, maximizing the anterior-posterior distribution of implants
- Cross-Arch Stabilization: Utilizing the arch form to resist rotational forces
- Cantilever Management: Minimizing or eliminating cantilevers, especially in compromised bone
Considerations in Compromised Sites
Maxillofacial defect cases often require modified biomechanical approaches:
- Strategic Implant Distribution: Maximizing support from available bone volumes
- Additional Implants: Sometimes necessary to compensate for compromised bone quality
- Specialized Implant Designs: Utilizing zygomatic, pterygoid, or angled implants
- Prosthesis Design Modifications: Adapting the prosthetic plan to work within biomechanical limitations
Specific Guidelines for Different Maxillofacial Regions
Implant positioning varies considerably depending on the specific region of the maxillofacial complex.
Maxillary Defect Reconstruction
In post-maxillectomy cases:
- Residual Alveolar Ridge: Primary site when available, often requiring careful spacing
-
Zygomatic Implants: Anchoring in the zygoma when maxillary bone is insufficient
- Standard Zygomatic Approach: Through the maxillary sinus
- Extramaxillary Technique: Lateral to the sinus in severe resorption cases
- Pterygoid Implants: Utilizing the pterygoid plate for posterior support
- Nasalfloor Implants: In select cases with adequate bone thickness
Mandibular Defect Reconstruction
Following mandibulectomy or trauma:
-
Reconstructed Areas: Implant placement in fibula, iliac crest, or scapular grafts
- Requires consideration of graft orientation and vascular pedicle
- Native Mandible: Strategic use of remaining bone, often with altered biomechanics
- Transitional Zones: Special attention at the junction between native and reconstructed bone
Orbital, Auricular, and Nasal Implants
For facial prosthesis support:
- Orbital Rim Implants: Typically supero-lateral and infero-lateral positions
- Auricular Implants: Usually in mastoid process, considering symmetry with contralateral ear
- Nasal Implants: Often in the glabella and maxillary/piriform regions
- Spacing Considerations: Typically 15-20mm between craniofacial implants for proper bar design
The Impact of Bone Quality and Quantity
Available bone volume and quality significantly influence implant positioning decisions.
Bone Classification Systems
Understanding bone quality helps predict success and guide technique modifications:
-
Lekholm and Zarb Classification:
- Type I: Homogeneous compact bone
- Type II: Thick cortical bone with dense trabecular core
- Type III: Thin cortical bone with dense trabecular bone
- Type IV: Thin cortical bone with low-density trabecular bone
-
Misch Bone Density Classification:
- D1: Dense cortical bone
- D2: Thick cortical with coarse trabecular bone
- D3: Thin cortical with fine trabecular bone
- D4: Minimal cortical with fine trabecular bone
Strategies for Compromised Bone
When ideal bone volume is unavailable, several approaches can be considered:
- Bone Augmentation: Through various grafting techniques
- Implant Size Modification: Using shorter or narrower implants when appropriate
- Alternative Positioning: Strategic placement in available bone stock
- Specialized Implants: Zygomatic, pterygoid, or angled designs
- Modified Surgical Protocols: Undersized preparation in soft bone, modified drilling sequences
Digital Planning for Precise Implant Positioning
Modern digital workflows have transformed the precision of implant planning and placement.
CBCT-Based Planning
Cone Beam Computed Tomography provides 3D visualization for optimal planning:
- Bone Volume Assessment: Accurate measurement of available bone
- Virtual Implant Placement: Testing various positions and angulations
- Anatomical Verification: Identifying and respecting vital structures
- Prosthetic Overlay: Combining bone data with prosthetic requirements
Digital Planning Software
Specialized software facilitates comprehensive treatment planning:
- Segmentation Capabilities: Isolating specific anatomical structures
- Implant Libraries: Including various implant designs and dimensions
- Prosthetic Design Tools: Visualizing the final restoration
- Collaborative Features: Allowing input from the entire treatment team
Guided Surgery Approaches
Transferring digital plans to the surgical field:
-
Static Guides: 3D-printed or milled surgical templates
- Fully Guided: Controlling depth, position, and rotation
- Partially Guided: Providing positional reference only
- Dynamic Navigation: Real-time tracking during surgery
- Robot-Assisted Surgery: Emerging technology for precise execution
Impression Techniques for Implant-Supported Maxillofacial Prosthetics
Accurate transfer of implant positions is critical for prosthesis fabrication.
Conventional Impression Methods
Traditional approaches still widely used:

-
Direct (Open Tray) Technique:
- Impression copings remain in the impression
- Preferred for multiple or angulated implants
- Process requires:
- Open tray impression copings fixed in mouth
- Custom tray with openings at implant sites
- Impression material applied with access to coping screws
- Screws loosened and impression removed with copings
- Lab analogs attached to replicate implant positions

-
Indirect (Closed Tray) Technique:
- Impression copings are removed and reattached to the impression
- Often used for simpler cases with favorable angulation
- Process involves:
- Closed tray impression copings attached
- Conventional impression made
- Impression removed leaving copings in mouth
- Copings removed and attached to analogs
- Assembly repositioned in impression
Digital Impression Methods
Increasingly adopted for accuracy and efficiency:
- Intraoral Scanning: Directly capturing implant positions with specific scan bodies
- Photogrammetry: Using multiple images to create accurate 3D representations
- CBCT Verification: Confirming implant positions through radiographic imaging
Special Considerations in Maxillofacial Cases
Modified approaches for complex defects:
- Sectional Impressions: For patients with limited opening
- Combined Techniques: Integrating conventional and digital approaches
- Custom Solutions: Modified impression copings for non-standard situations
Case Studies in Implant Positioning for Maxillofacial Prosthetics
Case 1: Post-Maxillectomy Rehabilitation
Clinical Situation: Hemimaxillectomy defect (Aramany Class II)
Challenge: Limited bone for implant placement, compromised biomechanics
Solution:
- Strategic placement of four implants in remaining anterior and posterior maxilla
- One zygomatic implant to provide posterior support
- Digital planning to optimize positions relative to anticipated load
Outcome: Successful obturator retention with improved function and comfort
Case 2: Mandibular Reconstruction with Fibula Graft
Clinical Situation: Segmental mandibulectomy reconstructed with fibula free flap
Challenge: Vertical discrepancy between fibula and native mandible, limited bone height
Solution:
- Virtual surgical planning of implant positions prior to reconstruction
- Strategic placement respecting the vascular pedicle
- Short implants in areas of limited vertical height
- Prosthetic design accommodating biomechanical limitations
Outcome: Fixed implant-supported prosthesis restoring form and function
Case 3: Auricular Prosthesis
Clinical Situation: Congenital microtia requiring ear prosthesis
Challenge: Determining optimal implant positions for aesthetic and functional outcomes
Solution:
- Mirror-image planning based on contralateral ear
- Strategic positioning of three craniofacial implants in the mastoid region
- Consideration of future hearing aid attachment
Outcome: Stable, aesthetic auricular prosthesis with integrated hearing solution
Training and Educational Considerations
Developing expertise in implant positioning for maxillofacial cases requires specialized education.
Learning Curve Elements
Key aspects of the learning process include:
- Anatomical Knowledge: Detailed understanding of standard and altered anatomy
- Case-Based Learning: Analysis of successful and failed cases
- Hands-On Experience: Supervised placement with increasing complexity
- Interdisciplinary Training: Exposure to prosthodontic, surgical, and technological aspects
NEET MDS Preparation
For students preparing for NEET MDS examinations:
-
Focus Areas:
- Implant treatment planning principles
- Anatomical considerations in standard and compromised situations
- Biomechanical concepts and force distribution
- Digital planning workflows
-
Recommended Resources:
- NEET Previous Year Question Papers: Review questions on implant positioning
- Maxillofacial Prosthodontics Books: Sections on treatment planning and implant surgery
- Flashcard Applications for NEET: Create specialized sets on implant positioning
- NEET Revision Tools: Create decision trees for implant placement scenarios
Common Complications Related to Implant Positioning
Improper implant positioning can lead to various complications, which clinicians must understand to prevent.
Aesthetic Complications
Positioning errors that compromise appearance:
- Visible Implant Components: Due to insufficient labial bone or improper depth
- Gingival Recession: From placing implants too far facially
- Asymmetric Emergence Profiles: Resulting from irregular spacing or angulation
- Crown Length Discrepancies: When implant depth is inconsistent
Functional Complications
Positioning errors affecting performance:
- Occlusal Interference: From improper positioning relative to opposing dentition
- Compromised Hygiene Access: When implants are placed too close together
- Speech Impairment: Particularly with anterior implants positioned incorrectly
- Food Impaction Areas: Created by improper emergence profiles
Mechanical Complications
Positioning errors leading to hardware problems:
- Screw Loosening: Often due to off-axis loading from poor positioning
- Component Fracture: From excessive force magnification due to improper positioning
- Prosthesis Instability: When implant distribution doesn't provide adequate support
- Excessive Wear: On components subjected to unfavorable forces
Biological Complications
Positioning errors affecting tissue health:
- Peri-implantitis: More common with implants placed with insufficient bone
- Bone Dehiscence: When implants are positioned too far facially
- Nerve Damage: From encroachment on vital anatomical structures
- Sinus Perforation Complications: When maxillary implants extend excessively into the sinus
Contemporary Trends and Future Directions
The field continues to evolve with several emerging approaches to implant positioning.
Computer-Assisted Dynamic Navigation
Real-time guidance systems offering:
- Flexibility: Adjustments possible during surgery
- Minimal Equipment: Less invasive than static guides
- Real-Time Feedback: Immediate verification of position
Robotic-Assisted Placement
Emerging technology providing:
- Sub-millimeter Precision: Exceeding human capabilities
- Tremor Elimination: Steady execution of the planned position
- Fatigue Reduction: Maintaining accuracy in lengthy procedures
AI-Enhanced Planning
Artificial intelligence applications offering:
- Automated Anatomy Recognition: Identifying critical structures
- Optimized Position Suggestions: Based on thousands of previous cases
- Outcome Prediction: Estimating success probability of proposed positions
Patient-Specific Implants
Custom-manufactured implants designed for specific anatomical situations:
- Defect-Matching Designs: Conforming to unique patient anatomy
- Integrated Attachment Features: Built-in connections for prostheses
- Biomimetic Properties: Surface and structural features optimized for specific sites
- Combined Reconstructive Elements: Integrating scaffolding and implant functions
Finding Care: The Implant and Oral Surgery Centre
For patients seeking specialized care in implant-supported maxillofacial rehabilitation, finding the right provider is crucial.
Specialized Treatment Centers
Several options exist for expert implant positioning in complex cases:
- University Dental Schools: Often leading research and innovation in complex implant cases
- The Implant and Oral Surgery Centre: Specialized facilities combining surgical and prosthetic expertise
- Maxillofacial Prosthodontics Fellowship centers: Institutions training the next generation of specialists
Provider Qualifications to Consider
When seeking care, look for clinicians with:
- Advanced training in both surgical and prosthetic aspects of implant therapy
- Experience with complex maxillofacial cases similar to your specific situation
- Access to modern digital planning and guided surgery capabilities
- Collaboration with multidisciplinary teams for comprehensive care
Conclusion: The Art and Science of Strategic Implant Positioning
The question of where does the implant go represents the critical foundation upon which successful maxillofacial rehabilitation is built. In the context of challenging maxillofacial defects, this decision becomes even more significant, requiring the clinician to balance anatomical limitations, biomechanical principles, and prosthetic requirements.
For students preparing for NEET MDS examinations, understanding these principles provides essential context for advanced prosthodontic concepts. For practicing clinicians, mastering the nuances of strategic implant positioning opens doors to providing life-changing reconstructive solutions for patients with complex maxillofacial needs.
As digital technologies continue to enhance our planning capabilities and surgical precision, the future holds tremendous promise for even more predictable and patient-specific approaches to implant positioning in maxillofacial prosthodontics.