Maxillofacial Prosthodontics and Implantology: The Synergistic Relationship
Medi Study Go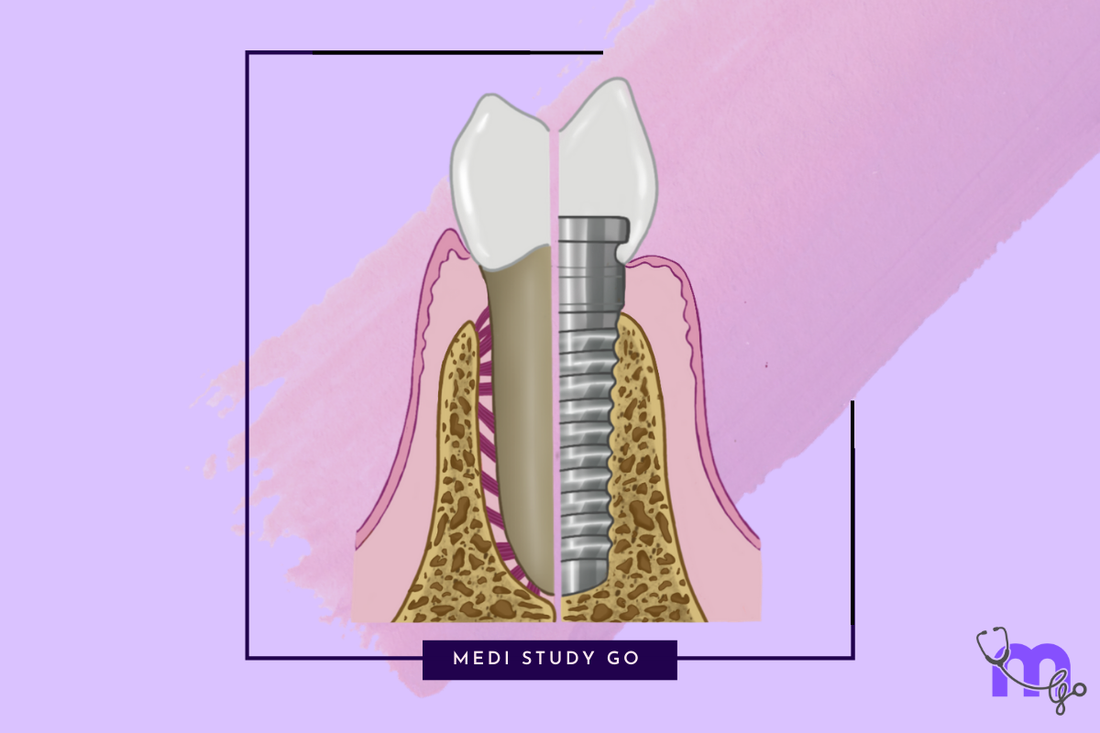
Related Resources:
- Understanding Maxillofacial Prosthodontics: Definition and Scope
- Implant Placement and Positioning: Where Does the Implant Go?
- Implant Retention and Stability: Effectiveness Without Pulling Out
- Advanced Techniques in Maxillofacial Prosthodontics
Introduction: A Revolutionary Partnership
The integration of implantology with maxillofacial prosthodontics represents one of the most significant advancements in rehabilitative dentistry of the past half-century. This powerful combination has transformed treatment possibilities for patients with maxillofacial defects, offering unprecedented levels of prosthetic stability, function, and aesthetics.
For students preparing for NEET MDS examinations, understanding the synergistic relationship between these two fields is essential for mastering advanced concepts in oral rehabilitation. For practicing clinicians, this knowledge opens doors to providing life-changing solutions for patients with complex maxillofacial needs.
"The marriage of implant technology with maxillofacial prosthodontics has rewritten what's possible in facial rehabilitation, offering hope to patients who previously had limited reconstructive options."
This article explores how maxillofacial prosthodontics and implantology complement each other, creating treatment possibilities that neither discipline could achieve independently.
The Evolution of Implants in Maxillofacial Rehabilitation
Historical Perspective
The journey toward integrating implants with maxillofacial prosthetics has been transformative:
1950s-1960s: Early experimentation with implant materials and designs, with limited success in maxillofacial applications.
1970s-1980s: Brånemark's osseointegration principles revolutionized implant dentistry, but applications in maxillofacial defects remained challenging.
1990s: Development of specialized implant systems specifically for craniofacial applications, including extraoral implants for facial prostheses.
2000s-Present: Advancements in digital planning, guided surgery, and prosthetic materials have made implant-supported maxillofacial rehabilitation increasingly predictable and accessible.
Impact on Patient Outcomes
The integration of implants has dramatically improved outcomes for maxillofacial patients in several key ways:
- Enhanced Quality of Life: Studies consistently demonstrate significant improvements in patient-reported quality of life with implant-retained prostheses compared to conventional alternatives.
- Psychological Benefits: The security and confidence provided by stable prostheses reduce social anxiety and improve psychological well-being.
- Functional Improvements: Implant-supported prostheses allow for improved speech, mastication, and swallowing function.
- Long-term Success: With proper maintenance, implant-supported maxillofacial prostheses demonstrate excellent longevity.

How Implants Enhance Maxillofacial Prosthetics
The clinical advantages of incorporating dental implants into maxillofacial rehabilitation are numerous and significant.
Improved Retention and Stability
Perhaps the most obvious benefit is the dramatic improvement in prosthesis retention:
- Elimination of Adhesives: Reducing daily maintenance and skin irritation for facial prostheses
- Mechanical Retention: Utilizing precision attachments between implants and prostheses
- Resistance to Dislodgement: Providing security during speaking, eating, and physical activities
- Consistent Positioning: Ensuring the prosthesis returns to the same position each time
Preservation of Anatomical Structures
Unlike conventional prostheses that may accelerate bone resorption through pressure:
- Bone Maintenance: Functional loading of implants helps preserve bone volume and density
- Protection of Remaining Teeth: Reducing the need to prepare adjacent teeth for retention
- Soft Tissue Health: Minimizing pressure on compromised tissues in post-surgical or irradiated sites
Enhanced Functional Capabilities
Implant-supported prostheses allow patients to regain function closer to pre-defect levels:
- Improved Bite Force: Studies show significantly higher masticatory efficiency with implant-supported versus conventional prostheses
- Speech Improvement: Better stability leads to more consistent articulation patterns
- Sensory Feedback: Rigid connection provides improved proprioception during function
Superior Aesthetics
The aesthetic advantages include:
- Elimination of Visible Retention Elements: No clasps or external fixation devices
- Better Support for Facial Contours: Preventing collapse of facial features
- Natural Transitions: Creating more imperceptible margins between prostheses and natural tissues
- Longevity of Appearance: Maintaining aesthetic results over time
Types of Implants Used in Maxillofacial Prosthodontics
Various implant systems serve different rehabilitation needs in the maxillofacial region.
Endosseous Dental Implants
Standard dental implants remain the workhorse for intraoral rehabilitation:
- Conventional Implants: Typically 3.75-4.2mm diameter, used in areas with adequate bone volume
- Small Diameter Implants: For narrow ridges or limited interdental spaces
- Short Implants: When vertical bone height is compromised
- Zygomatic Implants: For severe maxillary resorption, anchoring in the zygomatic bone
Craniofacial Implants
Specialized implants designed specifically for extraoral prosthesis retention:
- Shorter Length: Typically 3-5mm compared to dental implants
- Wider Platform: Providing broader connection surface for prosthetic attachments
- Flange Design: Often featuring a subperiosteal flange for additional stability
Attachment Systems
Various connection mechanisms link implants to maxillofacial prostheses:
- Bar-Clip Systems: Providing excellent stability and retention for larger prostheses
- Magnetic Attachments: Useful for patients with limited dexterity or when alignment is challenging
- Ball Attachments: Offering good retention with simpler design and maintenance
- Custom Abutments: For complex cases requiring precise angulation and emergence
Clinical Applications in Different Maxillofacial Defects
The implant-prosthetic connection benefits various maxillofacial rehabilitation scenarios.
Maxillary Defects
For patients with partial or complete maxillectomy:
- Strategic Implant Placement: Often in the remaining alveolar ridge, zygoma, or pterygoid regions
- Prosthetic Approach: Typically obturator prostheses or fixed implant-supported bridges
- Special Considerations: Managing limited bone volume and addressing sinus communication
Mandibular Defects
Following mandibulectomy or trauma:
- Implant Challenges: Often complicated by radiation history and reconstructive surgery
- Prosthetic Solutions: From partial dentures to full-arch fixed prostheses
- Occlusal Considerations: Managing deviation and achieving balanced force distribution
Facial Prostheses
For auricular (ear), nasal, orbital, or complex facial defects:
- Implant Positioning: Strategic placement to support specific prosthetic needs
- Number of Implants: Typically 2-4 implants per facial prosthesis
- Integration with Epitheses: Creating removable yet secure prosthetic connections
Combined Defects
For patients with extensive defects affecting multiple regions:
- Comprehensive Planning: Coordinating intraoral and extraoral implant placement
- Prosthetic Integration: Creating cohesive rehabilitation between different prosthetic components
- Phased Approach: Often necessary to address priorities in stages
The Impact of Radiation Therapy
Many maxillofacial patients undergo radiation treatment, which significantly impacts implant therapy.
Challenges in Irradiated Bone
Radiation creates several obstacles for successful implant treatment:
- Reduced Vascularity: Compromising healing and osseointegration
- Hypocellularity: Limiting regenerative capacity
- Fibrosis: Affecting soft tissue elasticity and surgical access
- Increased Osteoradionecrosis Risk: A serious complication that must be prevented
Evidence-Based Approaches
Research supports several strategies for improving outcomes:
- Timing Considerations: When possible, placing implants before radiation or waiting 12+ months after completion
- Hyperbaric Oxygen Therapy: May improve vascularity and osseointegration potential in select cases
- Modified Surgical Protocols: Gentler techniques, longer healing periods, antibiotic prophylaxis
- Alternative Implant Sites: Utilizing non-irradiated areas when available
Case Selection
Careful patient selection is crucial:
- Radiation Dosage: Higher success rates with cumulative doses below 50 Gy
- Patient Factors: Overall health, oral hygiene capability, compliance with follow-up
- Risk Assessment: Weighing benefits against potential complications
Digital Workflow in Implant Maxillofacial Prosthodontics
Modern digital technologies have transformed the planning and execution of implant therapy for maxillofacial defects.
Virtual Planning
Advanced software allows precise preoperative planning:
- 3D Reconstruction: Converting CT/CBCT data into virtual models
- Virtual Implant Placement: Optimizing position relative to available bone and prosthetic needs
- Prosthetic Simulation: Visualizing the final outcome before surgical intervention
Guided Surgery
Transferring the digital plan to the clinical situation:
- Stereolithographic Guides: 3D-printed surgical templates for precise implant placement
- Navigation Systems: Real-time tracking during surgery
- Robot-Assisted Surgery: Emerging technology for maxillofacial applications
CAD/CAM Prosthetics
Digital design and fabrication of the final prostheses:
- 3D Facial Scanning: Capturing detailed soft tissue topography
- Custom Abutment Design: Creating precise connections between implants and prostheses
- Direct Prosthesis Fabrication: Utilizing additive manufacturing for final or interim prostheses
Case Studies: Transformative Applications
Case 1: Post-Maxillectomy Rehabilitation
Patient Profile: 62-year-old male following right maxillectomy for squamous cell carcinoma
Challenge: Extensive defect creating oronasal communication, compromised speech, and facial collapse
Implant Solution: Four strategic implants placed in the remaining left maxilla and zygomatic region
Prosthetic Outcome: Bar-retained obturator prosthesis restoring speech, mastication, and facial support
Quality of Life Impact: Patient reported dramatic improvement in social confidence and nutritional intake
Case 2: Auricular Prosthesis
Patient Profile: 14-year-old female with congenital microtia (underdeveloped external ear)
Challenge: Creating a natural-appearing, stable ear prosthesis during adolescent growth
Implant Solution: Two craniofacial implants placed in the mastoid region
Prosthetic Outcome: Magnetically-retained silicone ear prosthesis with exceptional aesthetic match
Quality of Life Impact: Significant psychological benefit during critical developmental years
Case 3: Complex Facial Reconstruction
Patient Profile: 45-year-old male following extensive trauma from industrial accident
Challenge: Combined intraoral and extraoral defects requiring comprehensive rehabilitation
Implant Solution: Strategic implant placement for both dental and facial prosthesis support
Prosthetic Outcome: Integrated system of fixed dental prosthesis and removable facial components
Quality of Life Impact: Return to workplace and family life with restored function and appearance
Future Directions in Implant Maxillofacial Prosthodontics
Emerging technologies and approaches are poised to further advance this field.
Tissue Engineering and Regenerative Approaches
Moving beyond traditional implant-prosthetic connections:
- Growth Factor Applications: Enhancing bone regeneration around implants
- Stem Cell Therapies: Potential for rebuilding lost tissues rather than replacing them
- 3D-Printed Scaffolds: Custom structures for guided tissue regeneration
Material Innovations
Next-generation materials with improved properties:
- Surface Modifications: Promoting faster and more predictable osseointegration
- Biomimetic Materials: Prosthetics that more closely mimic natural tissues
- Smart Materials: Adaptive components that respond to changing conditions
Psychological and Functional Assessment
More sophisticated measurement of outcomes:
- Virtual Reality Testing: Assessing function in simulated environments
- Patient-Reported Outcome Measures: Standardized tools specific to maxillofacial rehabilitation
- Long-Term Tracking: Better understanding of lifetime outcomes
Educational Considerations for NEET MDS Preparation
For dental students preparing for NEET MDS examinations, several learning strategies are beneficial:
Key Focus Areas
- Implant Biomechanics: Understanding load distribution in compromised maxillofacial anatomy
- Treatment Planning Principles: Learning systematic approaches to complex cases
- Surgical-Prosthetic Coordination: Appreciating the interdisciplinary nature of care
- Complication Management: Recognizing and addressing potential problems
Recommended Resources
- NEET Previous Year Question Papers: Review questions specific to implant and maxillofacial topics
- NEET Preparation Books: Focus on sections covering implantology and maxillofacial prosthodontics
- Flashcard Application for NEET: Create specialized flashcards for this integrated topic
- NEET Mock Tests: Practice application of concepts in examination format
Advanced Study Techniques
- Case-Based Learning: Analyzing documented cases from the literature
- Visualization Exercises: Mentally working through treatment sequences
- Collaborative Discussion: Forming study groups to debate treatment approaches
- Revision Tools for NEET: Creating summary sheets of key principles
Finding Specialized Care
For patients seeking treatment combining maxillofacial prosthodontics and implantology, several resources exist:
Specialized Treatment Centers
- University Dental Schools: Often home to maxillofacial prosthodontic programs
- The Implant and Oral Surgery Centre: Specialized facilities combining surgical and prosthetic expertise
- Comprehensive Cancer Centers: Major hospitals with dedicated maxillofacial rehabilitation departments
Specialist Qualifications
When seeking care, look for providers with:
- Maxillofacial Prosthodontics Fellowship training
- Board Certification in prosthodontics
- Advanced Implant Training with maxillofacial applications
- Experience with Prosthodontics Oral Maxillofacial Surgery integration
Conclusion: The Future of Maxillofacial Rehabilitation
The synergistic relationship between maxillofacial prosthodontics and implantology has fundamentally transformed rehabilitation options for patients with some of the most challenging defects in healthcare. This integration represents not merely a technical advancement but a profound shift in what's possible for restoring both function and quality of life.
For students preparing for NEET MDS examinations, understanding this relationship provides essential context for advanced prosthodontic concepts. For practicing clinicians, the ongoing evolution of techniques and technologies in this field offers exciting possibilities to enhance patient care through innovation and evidence-based approaches.
As we continue to witness advancements in digital workflows, biomaterials, and interdisciplinary collaboration, the future of implant-supported maxillofacial prosthodontics holds tremendous promise for creating even more remarkable rehabilitative outcomes.