Glass Ionomer Cements: A Comprehensive Review
Medi Study Go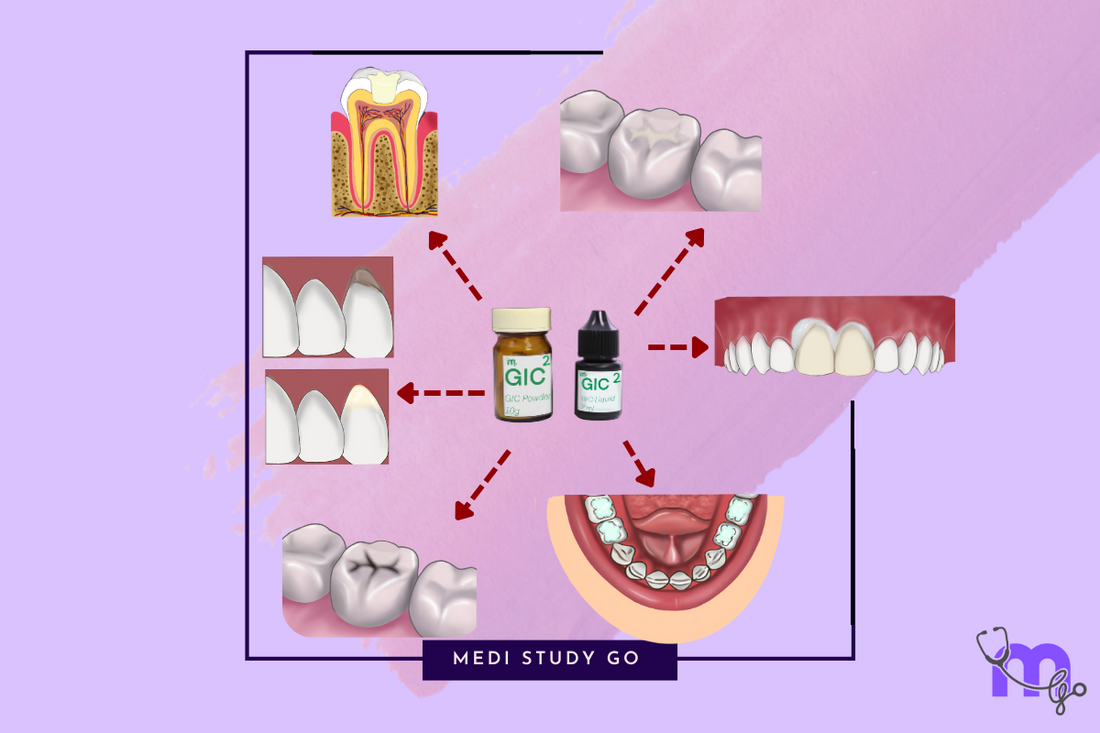
Introduction
Glass Ionomer Cements (GICs) represent one of the most versatile and widely used classes of dental materials. Since their introduction by Wilson and Kent in 1971, these cements have revolutionized numerous aspects of restorative and preventive dentistry.
Related Resources:
For NEET MDS aspirants, understanding the composition, properties, and clinical applications of GICs is essential for exam success and future clinical practice. This comprehensive guide explores conventional and modified glass ionomer cements, their setting reactions, and their significance in modern dentistry.
Composition of Glass Ionomer Cements
The unique properties of GICs stem from their specialized composition:
Powder Components
- Silica (SiO₂) - Primary glass-forming component
- Alumina (Al₂O₃) - Network modifier
- Calcium fluoride (CaF₂) - Source of fluoride release
- Sodium fluoride (NaF) - Additional fluoride source
- Aluminum phosphate (AlPO₄) - Contributes to structure
Liquid Components
- Polyacrylic acid - Bonds to enamel and dentin
- Tartaric acid - Improves handling, increases working time, shortens setting time
- Water - Medium for reaction and hydration
This composition allows GICs to bond chemically to tooth structure while providing fluoride release and biocompatibility, making them unique among dental materials.
Setting Reaction of Glass Ionomer Cements

The setting of GICs occurs in multiple distinct phases:
1. Leaching Phase (Ion Leaching)
- Acid attacks glass, releasing calcium, aluminum, and fluoride ions
- Initial gelation begins as ions are released into the aqueous medium
2. Hydrogel Phase
- Formation of initial calcium polyacrylate cross-links
- Material begins to set but remains weak and susceptible to contamination
3. Polysalt Gel Phase
- Aluminum ions continue cross-linking polyacrylic acid chains
- Final hardening occurs through formation of aluminum polyacrylate complex
- Silica gel forms around unreacted glass particles
This acid-base reaction results in a material with both ceramic and polymeric characteristics, giving GICs their unique properties.
Properties of Glass Ionomer Cements
GICs exhibit a combination of properties that make them suitable for various clinical applications:
Physical and Mechanical Properties
- Compressive strength: Approximately 150 MPa (weaker than composite resins)
- Tensile strength: 10-25 MPa
- Bond strength: 7.4 MPa to tooth structure
- Solubility: Low, but moisture-sensitive during initial setting
- Fluoride release: Provides long-term anticariogenic effect
- Thermal conductivity: Similar to natural tooth structure
Adhesion Properties
- Chemical bond: Forms calcium polyacrylate bonds with enamel and dentin
- Bond mechanism: Via carboxyl groups of polyacrylic acid
- No additional bonding agents required
- Mild self-etching effect: From polyacrylic acid
Biocompatibility
- Pulp response: Mild, generally well-tolerated
- pH changes: Initially acidic, gradually neutralizes
- Fluoride release: Sustained over time, with ability to be "recharged"
Classification of Glass Ionomer Cements
GICs can be classified according to their applications and composition. For NEET exam preparation, remember the mnemonic "Lazy Racoons Love Pizza On Couches, Having A Pancake":
Type 1 (L): Luting Cement
Used for cementing crowns, bridges, and orthodontic bands
Type 2 (R): Restorative Cement
For permanent restorations, particularly Class III and V cavities
Type 3 (L): Liners and Bases
Provides pulp protection and fluoride release
Type 4 (P): Pit and Fissure Sealants
Specialized formulations for preventive applications
Type 5 (O): Orthodontic Cement
For bonding brackets and bands
Type 6 (C): Core Build-up Material
Reinforced GIC used for large restorations
Type 7 (H): High Fluoride Releasing GIC
Enhanced fluoride release for high-caries-risk patients
Type 8 (A): Atraumatic Restorative Treatment
Formulated for the ART technique in field conditions
Type 9 (P): Pediatric GIC
Specifically designed for primary dentition
Modified Glass Ionomer Cements
Several modifications of conventional GICs have been developed to enhance specific properties:
1. Resin-Modified GIC (RMGIC)

Composition:
- Conventional GIC + light-curable resin (HEMA, Bis-GMA)
- Dual setting mechanism: acid-base reaction and polymerization
Advantages:
- Improved strength and wear resistance
- Reduced moisture sensitivity
- Faster initial setting (light-cured)
- Better bonding to composite resins
Uses:
- Restoration of class III and V cavities
- Liners, bases, and core build-ups
- Cementation of crowns, bridges, and orthodontic brackets
2. Metal-Modified GIC

Silver Alloy Admixed GIC
- "Miracle mix" - Spherical amalgam alloy powder mixed with Type II GIC
- Provides improved wear resistance
- Example: Ketac Silver
Cermet-Modified GIC
- Silver particles bonded to glass particles through sintering
- Higher fracture resistance
- Lower fluoride release
Uses:
- Small Class I restorations
- Core build-ups in grossly damaged teeth
3. High-Viscosity GIC
- Contains higher molecular weight polyacrylic acid
- Increased compressive strength and wear resistance
- Used primarily for atraumatic restorative treatment
4. Nano-Ionomer GIC
- Addition of nanoparticles (silica, zirconia) to GIC
- Provides better strength, polishability, and wear resistance
- Used in esthetic restorations and high-stress areas
Clinical Applications of Glass Ionomer Cements
The versatility of GICs is evident in their numerous clinical applications:
Restorative Applications
- Class V restorations: Particularly for cervical lesions
- Class III restorations: Where esthetics is not the primary concern
- Restoration of primary teeth: Especially Class I restorations
- ART technique: Field-based restorations in underserved areas
Preventive Applications
- Pit and fissure sealants: Especially in partially erupted teeth
- Preventive resin restorations: In combination with composite
- Fluoride-releasing restorations: For high-caries-risk patients
Cementation Applications
- Luting of metal crowns and bridges
- Cementation of orthodontic bands
- Implant abutment cementation
Other Applications
- Bases and liners: Under composite and amalgam restorations
- Core build-up: Especially with metal-reinforced variants
- Sandwich technique: In combination with composite resins
Sandwich Technique with Glass Ionomer Cements

The sandwich technique leverages the strengths of both GIC and composite resin:
Open Sandwich Te
chnique
- GIC is exposed to the oral environment (usually at the gingival margin)
- Typically used in Class V restorations where the cervical margin extends below the CEJ
- Benefits from fluoride release and chemical adhesion of GIC at the gingival margin
Closed Sandwich Technique
- GIC is completely covered by composite resin
- Used in deep dentin cavities where GIC provides a seal and pulp protection
- Indicated for Class I, II, and deep Class III cavities
- GIC not exposed to oral cavity
This technique combines the fluoride release and chemical adhesion of GIC with the superior esthetics and wear resistance of composite resins.
Manipulation and Clinical Tips

Proper handling of GICs is crucial for optimal clinical outcomes:
Powder-Liquid Mixing
- Hold liquid bottle vertically for accurate dispensing
- Dispense one level scoop of powder and two drops of liquid on a paper mixing pad
- Divide powder into two portions
- Incorporate first portion into liquid within 10 seconds
- Add second portion and mix thoroughly for 20-30 seconds
- Final mix should be glossy - loss of gloss indicates improper wetting
Capsulated Systems
- Pre-measured for consistent mixing
- Activate according to manufacturer's instructions
- Triturate for recommended time (usually 10 seconds)
- Use applicator gun for precise placement
Surface Protection
- Apply petroleum jelly or varnish to protect surface during initial setting
- Maintain moisture protection for at least 24 hours in conventional GICs
- For RMGICs, light-cure according to manufacturer's recommendations
Historical Development and Future Trends
Understanding the evolution of GICs can provide context for their current applications:
Key Historical Developments
- 1971: Wilson and Kent introduced ASPA I (first GIC)
- 1976: Modified form called ASPA II
- 1977: Miracle mix by GC America and Ketac Silver by 3M introduced
- 1980: First marketable cement (ASPA IV) and Vetrebond (first RMGIC)
- 1990: First light-cured GIC system
- 2007: Nano-ionomer technology by 3M
Future Directions
- Bioactive glass-containing GICs with remineralization capabilities
- Smart cements with controlled drug release properties
- Self-healing GICs with enhanced longevity
- Further improvements in strength and wear resistance
NEET Examination Tips for Glass Ionomer Cements
GICs are a popular topic in dental entrance examinations. Focus on these key areas:
High-Yield Topics for NEET
- Classification system: Know all nine types of GICs and their applications
- Setting reaction phases: Understand the three-phase setting mechanism
- Property comparisons: GIC vs. RMGIC vs. Composite resins
- Clinical applications: Which GIC type for which clinical situation
- Manipulation variables: How mixing affects properties
Common NEET Questions

- Composition differences between conventional GIC and RMGIC
- Fluoride release mechanism and clinical significance
- Setting reaction chemistry
- Indications and contraindications for different GIC types
- Sandwich technique applications
NEET Previous Year Questions (PYQs)
Review NEET previous year questions on GICs, focusing on:
- Classification systems
- Setting chemistry
- Clinical application scenarios
- Property comparisons with other cement types
Conclusion
Glass ionomer cements remain one of the most versatile materials in dentistry, offering unique advantages of chemical adhesion to tooth structure, fluoride release, and biocompatibility. Understanding their composition, properties, modifications, and applications is essential for NEET MDS preparation and clinical practice.
For dental students, mastering the manipulation of these materials will contribute significantly to successful restorative outcomes, while staying updated on the latest modifications and developments will ensure continued excellence in patient care.
