Calcium-Based Dental Cements: Clinical Applications
Medi Study Go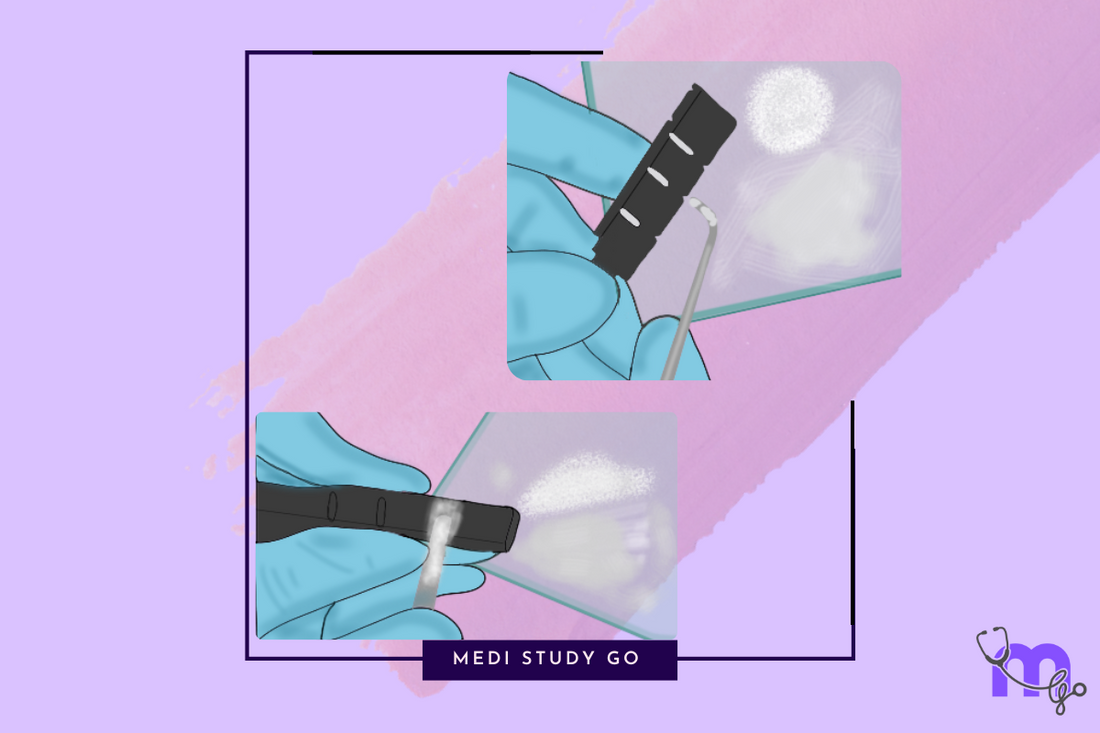
Introduction
Calcium-based dental cements have revolutionized various aspects of modern dentistry, particularly in areas related to pulp therapy, endodontics, and bioactive applications. These specialized materials play crucial roles in vital pulp therapy, perforation repair, and promoting healing of dental tissues.
Related Resources:
This comprehensive guide explores three key calcium-based dental cements: calcium hydroxide cement, mineral trioxide aggregate (MTA), and Biodentine, examining their composition, properties, and clinical applications essential for NEET MDS preparation.
Calcium Hydroxide Cement
Introduced by Herman in 1920, calcium hydroxide cement has been a cornerstone in vital pulp therapy for over a century.
Composition
Base Paste Components:
- Calcium hydroxide (main reactive ingredient)
- Zinc oxide (reinforcement)
- Calcium tungstate/Barium sulfate (radiopaque agent)
- Glycol salicylate (carrier)
Catalyst Paste Components:
- Calcium hydroxide
- Zinc oxide
- Zinc stearate (accelerator)
- Sulfonamide (carrier)
Setting Reaction
The setting reaction involves:
- Calcium disalicylate chelate formation
- Calcium hydroxide reacts with glycol salicylate
- Setting time: 2.5 to 5.5 minutes (accelerated by moisture)
Properties
- Compressive strength: 10-27 MPa (low)
- Tensile strength: 1.0 MPa (very low)
- Elastic modulus: 0.37 GPa
- Solubility: 0.4-7.8% (relatively high)
- pH: 9.2-11 (alkaline)
- Thermal conductivity: Provides some insulation
- Biocompatibility: Good, with antibacterial properties
- Therapeutic effect: Promotes reparative dentin formation
Clinical Applications
- Direct pulp capping - Applied directly to exposed vital pulp
- Indirect pulp capping - As a protective base in deep cavities
- Pulpotomy procedures - For partial removal of pulp tissue
- Temporary fillings - Intermediate restoration
- Base under restorations - Thermal insulation and pulp protection
Advantages and Disadvantages
Advantages:
- Antibacterial and alkaline nature
- Promotes secondary dentin formation
- Biocompatible with pulp tissues
- Compatible with composite restorations
- Radiopaque for monitoring
Disadvantages:
- Low compressive strength
- High solubility in oral fluids
- Brittle
- No adhesion to tooth structure
- Tunnel defects may form in reparative dentin
Mechanism of Action

Calcium hydroxide exerts its therapeutic effects through several mechanisms:
- Bacterial DNA damage (Imlay and Linn, 1988)
- Destruction of bacterial cytoplasmic membrane (Cotran et al., 1999)
- Protein lysis (Voet, 1995)
The highly alkaline pH leads to:
- Breakdown of ionic bonds of proteins
- Disturbance of biological activity of enzymes
- Cell membrane damage through lipid peroxidation
- Stimulation of pulp cells to form reparative dentin
Mineral Trioxide Aggregate (MTA)

Mineral Trioxide Aggregate represents a significant advancement in endodontic materials, offering superior sealing ability and biocompatibility.
Composition
MTA is essentially a modified Portland cement with the following components:
- Tricalcium silicate (66.1%) - Primary component
- Dicalcium silicate (8.4%)
- Tricalcium aluminate (2.0%)
- Tetracalcium aluminoferrite
- Calcium sulfate
- Bismuth oxide (14%) - For radiopacity
- Calcium oxide (8%)
- Silicon oxide (0.5%)
- Aluminum oxide (1%)
Types of MTA
Grey MTA:
- Contains iron oxide (FeO-present)
- Original formulation
- Slightly darker in color
White MTA:
- Iron oxide replaced with magnesium oxide (MgO)
- Matches hue of teeth better
- Developed for improved esthetics
Setting Reaction
The setting reaction involves:
- Hydration of calcium silicates
- Formation of calcium hydroxide
- Formation of calcium silicate hydrate
- CSH gel hardens
- Initial setting time: 3 hours for Grey MTA, 4 hours for White MTA
- Final pH: 12.5 (highly alkaline)
Properties
- Compressive strength: 40-50 MPa
- Initial setting time: 3-4 hours
- Final setting time: 24 hours
- pH: 12.5 (strongly alkaline)
- Radiopacity: High (for radiographic monitoring)
- Solubility: Low (ensures long-term stability)
- Biocompatibility: Excellent, bioactive, and tissue healing
Clinical Applications
- Pulp capping - Direct and indirect applications
- Pulpotomy/pulp regeneration - Promotes healing
- Perforation closure - Excellent sealing properties
- Root resorption closure - For internal or external resorption
- Root-end filling - For apicoectomy procedures
- Apexification - For immature teeth with open apices
Advantages and Disadvantages
Advantages:
- Superior sealing ability
- Biocompatible and bioactive
- Induces healing and new dentin formation
- Antibacterial properties
- Moisture tolerant
- Radiopaque for monitoring
Disadvantages:
- Long setting time
- Difficult handling
- Expensive compared to conventional cements
- Tooth discoloration (particularly with grey MTA)
- Potential genotoxicity (in some studies)
Biodentine
Introduced as a recent advancement in calcium silicate-based materials, Biodentine is marketed as a "bioactive dentin substitute" with improved handling properties compared to MTA.
Composition
Powder Components (packaged in 0.7g capsule):
- Tricalcium silicate (main core)
- Dicalcium silicate
- Calcium carbonate
- Iron oxide (for shade)
- Zirconium oxide (for radiopacity)
Liquid Components (packaged in 0.18ml pipette):
- Calcium chloride (accelerator)
- Hydrosoluble polymer (water-reducing agent)
- Water
Setting Reaction
The setting process involves:
- Hydration of calcium silicates
- Formation of calcium silicate gel
- Precipitation of calcium hydroxide
- Initial setting time: 6 minutes
- Final setting time: 10-12 minutes
Properties
- P ratio: 1 capsule powder to 5 drops liquid
- Manipulation: In amalgamator for 30 seconds
- Setting time: Initial (6 minutes), Final (10-12 minutes)
- Density: 2.26 g/cm³
- Porosity: 6.8%
- Compressive strength: 131.5 MPa (1hr), 241.1 MPa (24hr)
- Mechanical resistance: Higher than MTA
- Biocompatibility: Well-tolerated by body
- Bioactivity: Promotes formation of hydroxyapatite
- Low solubility: Contributes to longevity in dental applications
- Thermal conductivity: Low, provides good thermal insulation for pulp
Clinical Applications
- Dentine substitute under composite: Replaces lost dentin
- Direct pulp capping material: Excellent biocompatibility
- For perforations, apexification, and resorption: Endodontic repair
- Endodontic repair material: Seals defects in root canal system
Step-by-Step Procedure for Pulp Capping with Biodentine

- Proceed to caries excavation, first rinsing with 5% NaOCl
- Let the pulp appear and allow bleeding
- Control bleeding by applying a cotton pellet moistened with 5% NaOCl
- If bleeding control is achieved within 5 minutes, fill the cavity with Biodentine
- If not, remove part of the pulp (partial pulpotomy) and resume attempt to control bleeding
- Perform progressive pulpotomy until bleeding control is achieved
- When root canal entries are visible (full pulpotomy) and bleeding is controlled, fill with Biodentine
- If bleeding control within 5 minutes is impossible, perform root canal treatment
Advantages and Disadvantages
Advantages:
- Faster setting time than MTA
- High biocompatibility and pulp healing ability
- Strong mechanical properties
- Fluoride release for added protection
- Can be used as dentine substitute under composite
Disadvantages:
- Expensive compared to conventional cements
- Requires careful handling due to fast setting
- Technique sensitive
Comparison of Calcium-Based Cements
For NEET MDS preparation, understanding the comparative properties of these materials is essential:
| Property | Calcium Hydroxide | MTA | Biodentine |
|---|---|---|---|
| Setting time | 2.5-5.5 minutes | 3-4 hours | 6-12 minutes |
| Compressive strength | 10-27 MPa | 40-50 MPa | 131-241 MPa |
| Bioactivity | Moderate | High | Very high |
| Handling | Easy | Difficult | Moderate |
| Cost | Low | High | High |
| Primary use | Pulp capping | Endodontic repairs | Dentin substitute |
| pH | 9.2-11 | 12.5 | 12+ |
| Solubility | High | Low | Very low |
NEET Examination Tips for Calcium-Based Cements
Calcium-based dental cements are frequently tested in NEET MDS examinations. Focus on these high-yield aspects:
High-Yield Topics
- Composition differences: Know the key components of calcium hydroxide, MTA, and Biodentine
- Setting reactions: Understand the chemistry behind setting of each material
- Mechanical properties: Memorize comparative strength values
- Biological mechanisms: How these materials stimulate dentin bridge formation
- Clinical indications: When to use which material
- Historical development: Calcium hydroxide (1920), MTA (Portland cement modification), Biodentine (recent advancement)
Memory Aids
- MTA composition: Remember "TIPS" - Tricalcium silicate, Iron oxide (grey)/no iron (white), Portland cement basis, Silica
- Calcium hydroxide mechanism: "ABCD" - Alkaline pH, Bacterial inhibition, Cellular stimulation, Dentin bridge formation
- Biodentine properties: "FAST" - Fast setting, Aesthetic (tooth-colored), Strong mechanically, Treatment versatility
NEET PYQ Focus Areas
- Comparative properties between calcium-based materials
- Clinical applications and case-based questions
- Setting reaction chemistry
- Historical development questions
- Handling characteristics and manipulation variables
Recent Advancements and Future Trends
The field of calcium-based dental cements continues to evolve:
Recent Innovations
- MTA modifications: Faster-setting variants
- Nano-modified calcium silicate cements: Enhanced properties
- Calcium phosphate-incorporating materials: Improved bioactivity
- Light-curable calcium hydroxide formulations: Better handling
- Bioactive glass-containing calcium-based materials: Remineralizing potential
Future Directions
- Development of injectable calcium-based materials
- Smart materials with controlled drug release
- Combination materials with enhanced antibacterial properties
- Materials with improved handling and mechanical properties
- Customizable setting times for different clinical applications
Conclusion
Calcium-based dental cements represent a critical category of materials in modern dentistry, providing solutions for maintaining pulp vitality, repairing endodontic defects, and promoting healing of dental tissues. From the traditional calcium hydroxide cements to cutting-edge materials like MTA and Biodentine, these bioactive materials continue to evolve and improve clinical outcomes.
For NEET MDS aspirants, understanding the composition, properties, and applications of these materials is essential for exam success. The biological interactions and therapeutic potential of calcium-based cements make them one of the most fascinating topics in dental materials science, with ongoing research promising even more advanced formulations in the future.