Dental Cements: The Complete Guide for NEET and Dental Students
Medi Study Go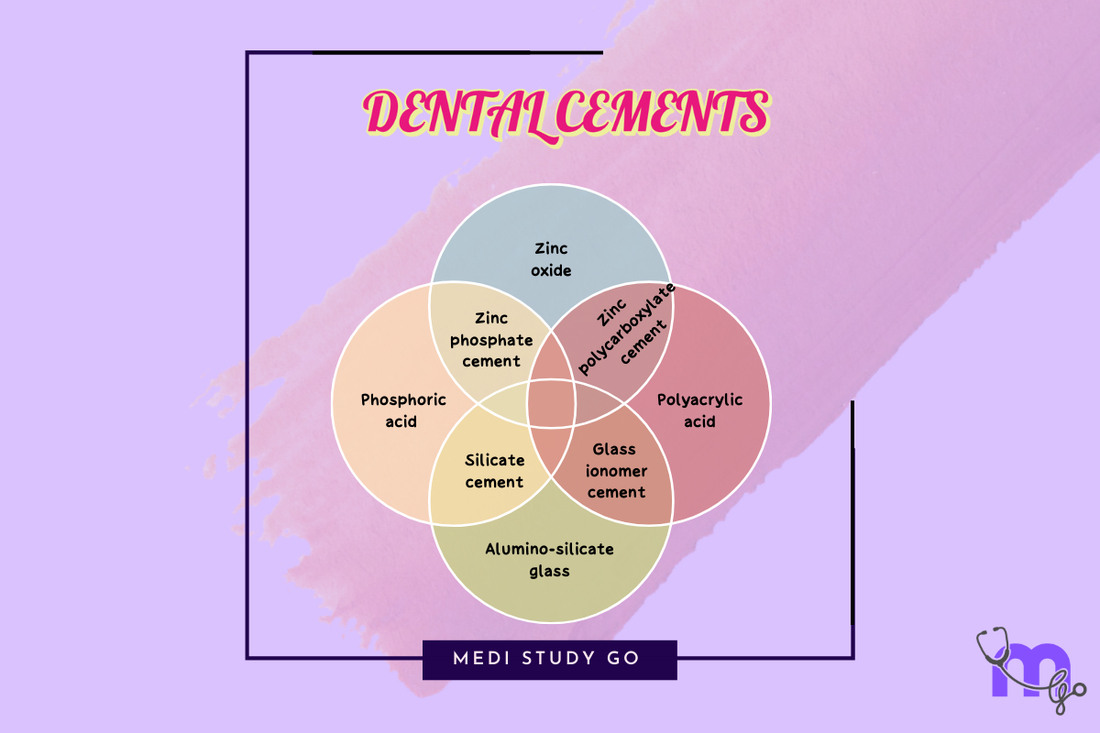
Introduction to Dental Cements
Dental cements are the unsung heroes of modern dentistry, playing a crucial role in various dental procedures and restorations. Whether you're a dental student preparing for your NEET MDS examination or a practicing dentist looking to refresh your knowledge, understanding dental cements is essential for providing quality dental care.
Related Resources:
In this comprehensive guide, we'll explore the fundamentals of dental cements, their classification, properties, clinical applications, and proper handling techniques. Whether you're studying for the NEET exam or looking to enhance your clinical knowledge, this resource will serve as your go-to reference for all things related to dental cements.
What Are Dental Cements?
Dental cements are specialized materials used in dentistry to bond or seal dental restorations, orthodontic appliances, and other dental materials to natural tooth structures. They serve as the critical interface between the restoration and the tooth, providing retention, sealing abilities, thermal insulation, and in some cases, therapeutic benefits.
These versatile materials function as:
- Luting agents - For permanent or temporary cementation of crowns, bridges, inlays, onlays, and orthodontic bands
- Cavity liners - Providing protection to the pulp from chemical, thermal, and mechanical irritants
- Base materials - Supporting restorations and providing thermal insulation
- Temporary or permanent restorative materials - For various clinical applications
- Pulp capping agents - Promoting pulp healing and dentin formation
- Root canal sealers - For endodontic treatments
History and Evolution of Dental Cements
The journey of dental cements began with simple materials and has evolved into sophisticated formulations designed for specific clinical applications.
Timeline of Key Developments:
- 1870s: Introduction of zinc phosphate cement, one of the oldest dental cements
- 1920: Introduction of calcium hydroxide cement by Herman
- 1971: Wilson and Kent introduced glass ionomer cement (ASPA I)
- 1976: Modified form of ASPA I named ASPA II
- 1977: Introduction of Miracle mix by GC America and Ketac Silver by 3M
- 1980s: Development of resin-modified cements
- 1990s: Advent of light-cured glass ionomer cements
- 2000s onwards: Nanotechnology incorporation and bioactive cement formulations
This evolution reflects the continuous pursuit of materials with improved properties, handling characteristics, and biological compatibility, demonstrating how dental cement technology continues to advance to meet clinical needs.
Classification of Dental Cements

Dental cements can be classified based on various parameters, including their composition, setting reaction, and clinical applications. Understanding this classification is crucial for NEET exam preparation and clinical decision-making.
Based on Composition
-
Zinc-based Cements
- Zinc phosphate cement
- Zinc oxide eugenol (ZOE) cement
- Zinc polycarboxylate cement
-
Glass-based Cements
- Glass ionomer cement (GIC)
- Resin-modified glass ionomer cement (RMGIC)
-
Resin-based Cements
- Self-adhesive resin cement
- Dual-cure resin cement
- Self-cure resin cement
- Light-cure resin cement
-
Calcium-based Cements
- Calcium hydroxide cement
- Mineral trioxide aggregate (MTA)
- Biodentine
Based on Setting Reaction
-
Acid-base Reaction Cements
- Zinc phosphate cement
- Zinc polycarboxylate cement
- Glass ionomer cement
-
Resin Polymerization Cements
- Composite cements
- Resin cements
Based on Function
-
Luting Cements
- Used for crown and bridge cementation
- Examples: Zinc phosphate, GIC, Zinc polycarboxylate, Resin cement
-
Restorative Cements
- Used for direct restorations
- Examples: GIC, RMGIC, Resin cement
-
Base/Liner Cements
- Used as protective barriers
- Examples: Calcium hydroxide, ZOE, GIC
-
Temporary Cements
- For provisional restorations
- Examples: Zinc oxide eugenol, Non-eugenol temporary cements
Properties of Ideal Dental Cements
The effectiveness of a dental cement depends on its physical, mechanical, and biological properties. An ideal dental cement should possess the following characteristics:
Physical Properties
- Low film thickness: Ensures proper seating of restorations (typically 25μm for luting cements)
- Low solubility: Prevents disintegration in oral fluids
- Adequate working and setting time: Allows manipulation and placement
- Good flowability: Facilitates complete coverage of restoration margins
- Thermal conductivity: Similar to natural tooth structures to provide insulation
Mechanical Properties
- High compressive strength: To withstand occlusal forces
- Adequate tensile strength: To resist fracture under tension
- Dimensional stability: Minimal expansion or contraction after setting
- Adhesion: Strong bonding to both tooth structure and restorative materials
Biological Properties
- Biocompatibility: Non-irritating to pulp and surrounding tissues
- Antibacterial activity: Prevents secondary caries
- Radiopacity: Visible on radiographs for monitoring
- Fluoride release: Provides anticariogenic benefits (in some cements like GIC)
Understanding these properties is crucial for selecting the appropriate cement for specific clinical situations and is a frequent topic in NEET MDS question papers.
Clinical Applications of Dental Cements
The versatility of dental cements is evident in their wide range of clinical applications:
1. Luting Applications
- Cementation of crowns and bridges
- Fixation of inlays and onlays
- Cementation of orthodontic bands and brackets
- Implant abutment cementation
2. Protective Applications
- Cavity liners to protect the pulp
- Bases under restorations
- Pulp capping materials
- Thermal insulation beneath metallic restorations
3. Restorative Applications
- Temporary fillings
- Core build-ups in grossly decayed teeth
- Atraumatic restorative treatments (ART)
- Pediatric restorations
4. Specialized Applications
- Root canal sealers
- Root-end filling materials
- Perforation repair materials
- Apexification procedures
Selecting the appropriate cement for a specific clinical situation requires consideration of factors such as:
- Required strength and durability
- Esthetic considerations
- Moisture control possibilities
- Patient's caries risk
- Restoration material compatibility
Dispensing and Mixing Techniques for Dental Cements
Proper dispensing and mixing of dental cements are critical for achieving optimal properties and clinical success. Different cement systems require specific handling techniques:
Powder-Liquid Systems
Most traditional cements like zinc phosphate, glass ionomer, and zinc polycarboxylate come in powder-liquid formulations.
Dispensing Steps:
- Hold liquid bottle vertically to ensure accurate drop size
- Dispense required number of drops onto a cool, clean glass slab
- Use the manufacturer's scoop to measure powder with a level scoop (avoid compacting)
- Follow the recommended powder-to-liquid ratio precisely
Mixing Techniques:
- Use a clean, dry agate spatula
- For most cements, incorporate powder into liquid in small increments
- Use broad, firm strokes to mix thoroughly
- Complete mixing within the manufacturer's specified time
- Achieve the desired consistency based on the intended application
Paste-Paste Systems
Resin cements and some temporary cements come in two paste components that must be mixed in equal proportions.
Dispensing and Mixing:
- Dispense equal lengths of base and catalyst pastes
- Mix thoroughly with a plastic spatula until a homogeneous color is achieved
- Mix rapidly within the working time to avoid premature setting
Capsulated Systems
Modern cement systems often come in pre-measured capsules for consistent mixing.
Procedure:
- Activate the capsule according to manufacturer's instructions
- Place in an amalgamator or triturator
- Mix at the recommended speed and time
- Apply directly from the capsule using the applicator
Common Mixing Errors to Avoid
- Incorrect powder-to-liquid ratio
- Inadequate mixing time or technique
- Mixing on an inappropriate surface (too warm or contaminated)
- Adding powder too quickly, resulting in inhomogeneous mix
- Delayed application after mixing, exceeding working time
Proper manipulation is essential for achieving the cement's intended properties and is a key factor in the long-term success of dental restorations.
Latest Advancements in Dental Cements
The field of dental cements continues to evolve with technological advancements and research. Recent innovations include:
Bioactive Cements
Modern cements that interact with tooth structures to promote remineralization and healing. Examples include:
- Calcium silicate-based cements
- Bioactive glass-containing cements
- Cements with remineralizing capabilities
Nanotechnology in Dental Cements
Incorporation of nanoparticles has led to improved properties:
- Nano-filled resin cements with enhanced strength
- Nano-ionomer technology (introduced by 3M in 2007)
- Silver nanoparticle-incorporated GIC with antibacterial properties
Self-Adhesive Systems
Single-step cements that eliminate the need for separate etching and bonding:
- Self-adhesive resin cements
- Universal cements with multi-substrate compatibility
These advancements represent the cutting edge of dental materials science and are shaping the future of restorative and prosthetic dentistry.
NEET Exam Preparation Tips for Dental Cements
The topic of dental cements is a favorite in NEET MDS and other dental entrance examinations. Here are some focused study strategies:
High-Yield Topics
- Classification systems of dental cements
- Setting reactions of different cement types
- Comparative properties of various cements
- Indications and contraindications
- Manipulation techniques and variables affecting cement properties
Exam Preparation Strategies
- Create comparison charts: Compare properties, advantages, and disadvantages of different cements
- Practice numerical questions: Film thickness, setting time, compressive strength values
- Memorize key dates: Historical development of dental cements
- Focus on clinical applications: Which cement for which scenario
- Review previous year questions: NEET PYQs often repeat core concepts
Memory Aids
For Glass Ionomer Cement classification, remember the mnemonic: "Lazy Racoons Love Pizza On Couches, Having A Pancake" for Types 1-9:
- L: Luting Cement
- R: Restorative cement
- L: Liners and Bases
- P: Pit and fissure sealants
- O: Orthodontic cement
- C: Core build-up material
- H: High fluoride releasing GIC
- A: Atraumatic restorative treatment
- P: Paediatric GIC
Conclusion
Dental cements are fundamental materials in modern dentistry, serving various purposes from luting to therapeutic applications. Their proper selection and manipulation are critical skills for any dental professional. As materials science advances, we can expect continued innovation in dental cement technology, further expanding their capabilities and applications.
Whether you're preparing for your NEET MDS examination or enhancing your clinical knowledge, a strong understanding of dental cements will serve as a solid foundation for your dental practice.