TMJ Anatomy and Function
Medi Study Go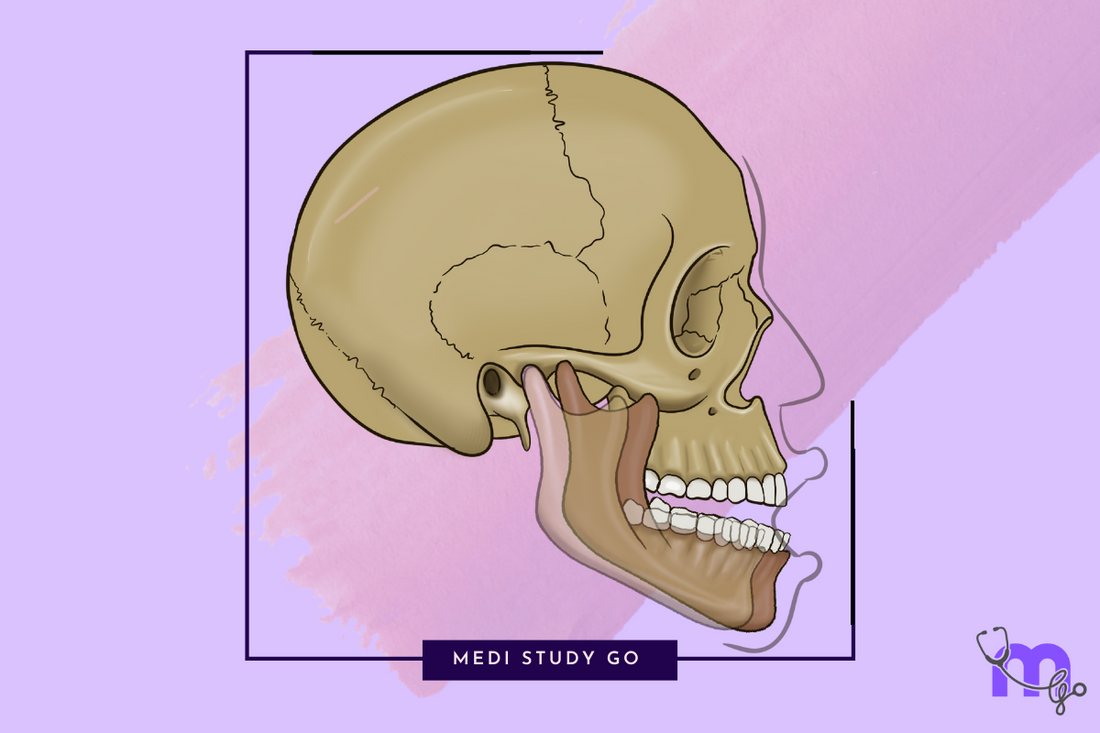
Structural Components of the Temporomandibular Joint
Related Resources
- Comprehensive Overview of TMJ Disorders
- Diagnosis of TMJ Disorders
- Non-Surgical Management of TMJ Disorders
- Surgical Management of TMJ Disorders
- Recovery, Complications and Advances in TMJ Treatment
The temporomandibular joint (TMJ) represents one of the most complex articulations in the human body, classified as a ginglymoarthrodial joint—combining hinge-like (ginglymoid) and gliding (arthrodial) movements. This unique joint consists of several key anatomical components that work in harmony to facilitate mandibular movement.
Articulating Surfaces
The TMJ forms where the mandibular condyle articulates with the mandibular fossa and articular eminence of the temporal bone. Unlike most synovial joints, the articulating surfaces of the TMJ are covered with fibrocartilage rather than hyaline cartilage, providing enhanced resistance to compressive forces during mastication.
Articular Disc

The articular disc (meniscus) serves as a crucial non-vascularized, dense fibrous connective tissue structure dividing the joint into two distinct compartments:
- Superior (meniscotemporal) compartment – Primarily facilitates translational movements
- Inferior (meniscomandibular) compartment – Responsible for rotational movements
The disc consists of three regions:
- Anterior band
- Intermediate zone (thinnest region)
- Posterior band (thickest region)
This biconcave structure accommodates the convex surfaces of the condyle and articular eminence, enhancing joint stability during movement.
Joint Capsule
The TMJ capsule is a fibrous envelope that surrounds the joint and attaches to the temporal bone superiorly and the condylar neck inferiorly. This capsule is:
- Reinforced laterally by the temporomandibular ligament
- Relatively thin anteromedially where the lateral pterygoid muscle attaches
- Lined internally by synovial membrane that produces synovial fluid
Supporting Structures of the TMJ
Ligaments Associated with TMJ
Several ligaments provide stability and guide movement of the temporomandibular joint:
- Temporomandibular Ligament – The primary lateral stabilizer, limiting posterior movement of the condyle and excessive mouth opening
- Sphenomandibular Ligament – An accessory ligament running from the spine of the sphenoid to the lingula of the mandible
- Stylomandibular Ligament – Extending from the styloid process to the angle of the mandible
- Capsular Ligament – Surrounds the joint and contains proprioceptive nerve endings that provide feedback on joint position
Muscles Involved in TMJ Movement
The coordinated action of several muscles enables the complex movements of the TMJ:

-
Muscles of Mastication
- Masseter – Powerful elevator of the mandible
- Temporalis – Elevates and retracts the mandible
- Medial Pterygoid – Elevates and protrudes the mandible
-
Lateral Pterygoid:
- Superior head – Stabilizes the condyle and disc during mouth closure
- Inferior head – Protrudes the mandible and assists in opening
-
Accessory Muscles
- Digastric – Assists in mandibular depression
- Mylohyoid – Elevates the floor of the mouth and assists in early phases of opening
- Geniohyoid – Works with suprahyoid muscles in mandibular depression
Neurovascular Supply of the TMJ
Blood Supply of TMJ
The rich vascular network supplying the TMJ includes:
- Superficial temporal artery
- Middle meningeal artery
- Maxillary artery (particularly the auricular deep branches)
- Masseteric artery
This extensive blood supply ensures proper nutrition and healing potential of the joint structures.
Nerve Supply of TMJ
The TMJ receives innervation primarily from the mandibular branch (V3) of the trigeminal nerve through:
- Auriculotemporal nerve (primary sensory supply)
- Masseteric nerve
- Deep temporal nerves
These nerves provide both sensory feedback and proprioceptive information essential for coordinated movement.
Functional Biomechanics of the TMJ

The TMJ facilitates several movement patterns crucial for mastication, speech, and facial expression:
- Depression and Elevation – Opening and closing of the mouth
- Protrusion and Retrusion – Forward and backward movement of the mandible
- Lateral Excursion – Side-to-side movement
These movements occur through a combination of rotation and translation:
- Rotation occurs primarily in the inferior joint compartment
- Translation occurs mainly in the superior joint compartment
During normal mouth opening, the initial 20-25mm of opening involves primarily rotation, while further opening requires translation of the condyle-disc complex along the articular eminence.
Histological Features of the TMJ
The TMJ exhibits unique histological characteristics:
- Fibrocartilage covering articular surfaces rather than hyaline cartilage
- Four distinct layers in the articular surfaces:
- Fibrous articular layer (superficial)
- Proliferative zone (intermediate)
- Fibrocartilaginous layer
- Calcified cartilage layer (deep)
Developmental Aspects of the TMJ
The TMJ develops later than most other joints in the body, with key developmental stages:
- Formation begins around the 8th week of embryonic life
- The temporomandibular joint is the last joint to develop in the body
- Development continues through adolescence with adaptive remodeling throughout life
Clinical Relevance of TMJ Anatomy
Understanding TMJ anatomy provides the foundation for recognizing pathological conditions:
- Disc displacement disorders often relate to attachments of the lateral pterygoid muscle
- Degenerative changes typically affect the fibrocartilaginous surfaces
- Myofascial pain often involves the muscles of mastication
- Growth abnormalities can affect joint development and function
