Non-Surgical Management of TMJ Disorders
Medi Study Go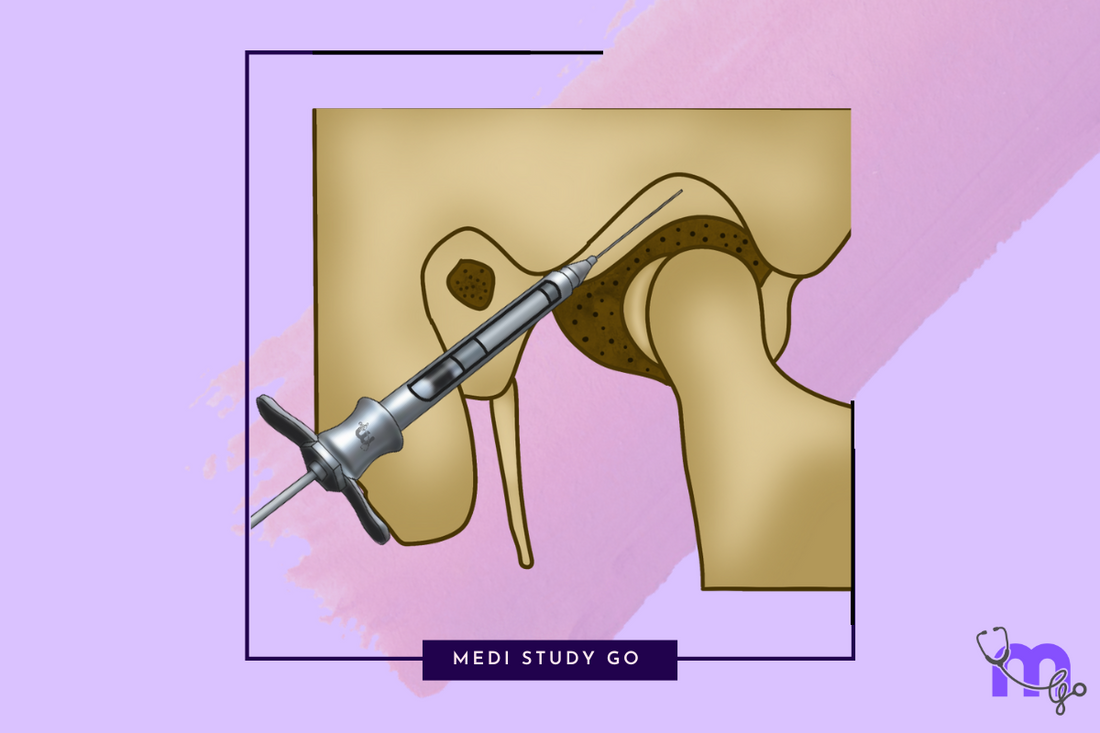
The Conservative Treatment Paradigm
Related Resources
- Comprehensive Overview of TMJ Disorders
- TMJ Anatomy and Function
- Diagnosis of TMJ Disorders
- Surgical Management of TMJ Disorders
- Recovery, Complications and Advances in TMJ Treatment
Non-surgical management represents the cornerstone of TMJ disorder treatment, with approximately 80-90% of patients experiencing significant improvement through conservative measures alone. The underlying philosophy embraces a minimally invasive approach, focusing on symptom management, functional restoration, and addressing contributing factors while allowing the body's adaptive capacity to facilitate healing.
Patient Education and Self-Care
Understanding and Behavioral Modification
Effective management begins with patient education regarding:
- The nature and prognosis of their specific TMJ condition
- Functional anatomy and biomechanics in lay terms
- Identification and avoidance of parafunctional habits
- Stress management techniques
- Sleep hygiene practices
Self-Care Protocols
Simple yet effective self-care measures include:
- Application of moist heat for muscle relaxation
- Cold therapy for acute inflammation
- Soft diet modifications to reduce joint loading
- Conscious relaxation of masticatory muscles
- Proper posture maintenance, especially during computer use
- Avoidance of extreme jaw movements (wide yawning, gum chewing)
Pharmacological Management
Analgesics and Anti-inflammatory Medications
- NSAIDs (Ibuprofen, Naproxen) – First-line medications for pain and inflammation
- Acetaminophen – Alternative for pain control when NSAIDs are contraindicated
- Topical analgesics – Containing capsaicin or compounded medications for localized pain
Muscle Relaxants
- Centrally acting (Cyclobenzaprine, Baclofen) – For acute muscle spasm, typically prescribed for short-term use (2-3 weeks)
- Benzodiazepines (Diazepam) – For severe cases with anxiety component, used cautiously due to dependency concerns
Adjunctive Medications
- Tricyclic antidepressants (Amitriptyline, Nortriptyline) – For chronic pain management at lower doses than used for depression
- Anticonvulsants (Gabapentin, Pregabalin) – For neuropathic pain components
- Botulinum toxin injections – For refractory myofascial pain with localized hypertrophy or persistent spasm
Physical Therapy Interventions
Manual Therapy Techniques
- Massage therapy – For myofascial trigger point deactivation
- Mobilization – Gentle joint mobilization to improve range of motion
- Stretching exercises – To reduce muscle tension and improve flexibility
- Postural correction – Addressing cervical and thoracic alignment issues
Therapeutic Modalities
- Ultrasound therapy – Deep tissue heating to enhance blood flow
- Transcutaneous Electrical Nerve Stimulation (TENS) – For pain modulation based on gate control theory
- Low-level laser therapy – To reduce inflammation and promote tissue repair
- Iontophoresis – Transdermal delivery of anti-inflammatory medications
Exercise Programs
- Controlled jaw opening exercises – To improve range of motion
- Isometric exercises – To strengthen masticatory muscles without joint movement
- Proprioceptive training – To improve neuromuscular coordination
- Postural exercises – Targeting cervical spine and shoulder girdle
Occlusal Appliance Therapy
Types of Occlusal Splints
-
Stabilization Splints (Michigan Splint)
- Provides stable and even occlusal contacts
- Reduces muscle hyperactivity
- Promotes neuromuscular harmony
- Typically worn at night
-
Anterior Repositioning Appliances
- Positions mandible forward
- Primarily for disc displacement with reduction
- Maintains condyle-disc relationship
- Usually transitional therapy
-
Posterior Bite Planes
- Increases vertical dimension
- Reduces joint loading
- Decreases muscle activity
Mechanism of Action
Occlusal appliances function through several mechanisms:
- Redistribution of occlusal forces
- Reduction of parafunctional activity
- Muscle relaxation and reprogramming
- Alteration of condylar position
- Placebo effect (estimated at 30-40% of therapeutic benefit)
Protocol for Splint Therapy
- Initial adjustment period of 2-4 weeks
- Regular follow-up for adjustments
- Assessment of symptomatic improvement
- Gradual weaning when symptoms resolve
- Consideration of definitive occlusal therapy if indicated
Psychological and Behavioral Interventions
Cognitive Behavioral Therapy (CBT)
CBT addresses psychological factors contributing to TMJ disorders through:
- Identification of pain-perpetuating thoughts and behaviors
- Development of adaptive coping strategies
- Stress management techniques
- Pain acceptance frameworks
Biofeedback
This technique enables patients to:
- Recognize masticatory muscle tension
- Learn voluntary control over muscle activity
- Reduce parafunctional habits
- Measure progress objectively
Relaxation Training
Various modalities include:
- Progressive muscle relaxation
- Diaphragmatic breathing exercises
- Mindfulness meditation
- Guided imagery
Acupuncture and Complementary Approaches
Traditional and Modern Acupuncture
- Traditional Chinese Medicine approaches
- Western medical acupuncture targeting trigger points
- Electroacupuncture for enhanced stimulation
- Typically requires 6-8 sessions for maximum benefit
Other Complementary Approaches
- Massage therapy targeting masticatory and cervical muscles
- Herbal anti-inflammatory supplements (with caution regarding evidence)
- Nutritional counseling to reduce inflammatory dietary components
Multidisciplinary Management Approaches
Team-Based Care
Optimal management often involves coordination between:
- Dental professionals
- Physical therapists
- Pain specialists
- Psychologists
- Otolaryngologists (when ear symptoms predominate)
- Neurologists (for complex pain presentations)
Staged Treatment Protocol
A typical protocol progresses through:
- Initial self-management and education
- Professional physical therapy and splint therapy
- Pharmacological intervention as needed
- Psychological support for chronic cases
- Consideration of minimally invasive procedures (arthrocentesis, arthroscopy)
- Surgical intervention only when conservative measures fail
When to Consider Surgical Management
Non-surgical approaches should be considered first-line therapy for most TMJ disorders. However, certain conditions warrant earlier consideration of surgical management:
- Confirmed degenerative joint disease with mechanical interference
- Ankylosis (fibrous or bony)
- Recurrent or chronic dislocation
- Developmental disorders affecting joint structure
- Neoplastic processes involving the TMJ
- Fractures with displacement affecting function