Pediatric and Infant CPR: Special Considerations
Medi Study Go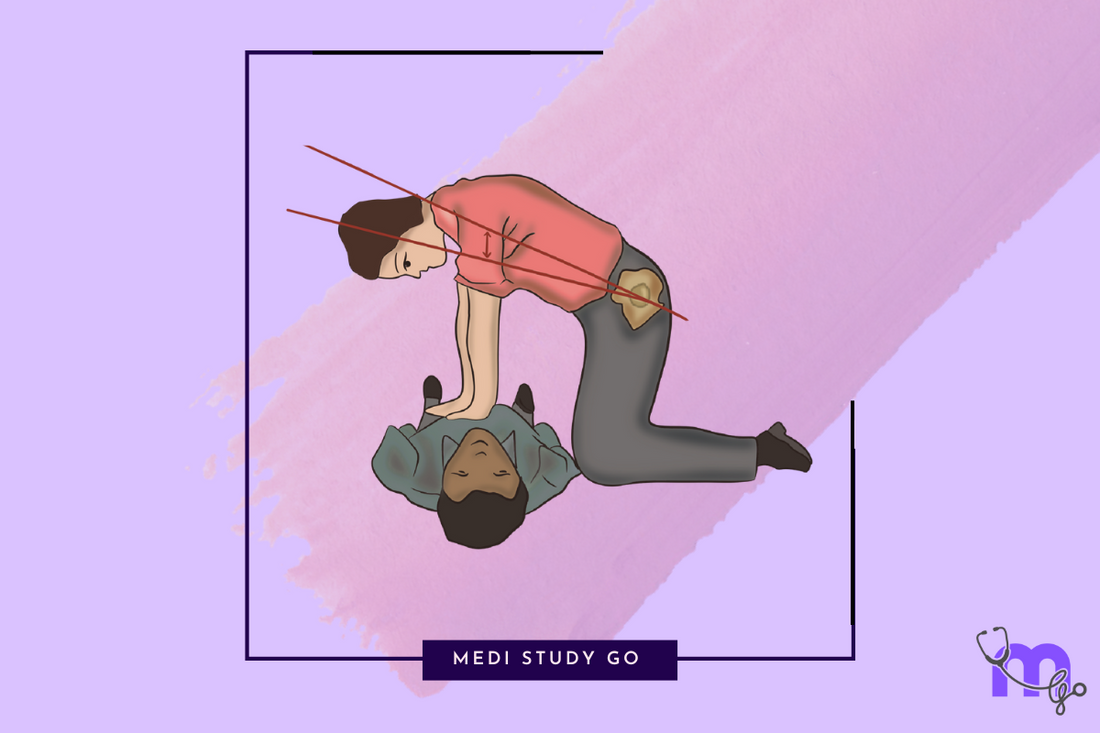
Master the essential differences in CPR techniques for children and infants. This guide is crucial for healthcare providers, NEET exam preparation, and anyone responsible for child safety.
Related CPR Resources
- Comprehensive Guide to Cardiopulmonary Resuscitation
- Adult CPR Techniques and Procedures
- CPR for Cardiac Emergencies and Heart Attacks
- AED Integration with CPR
- CPR Training and Certification
Understanding Pediatric and Infant CPR: Why It's Different
Cardiopulmonary resuscitation for children and infants follows different protocols than adult CPR due to anatomical, physiological, and causal differences. According to current CPR guidelines, these adaptations are critical for effective emergency response.
For medical students preparing for NEET MDS and other examinations, understanding these distinctions is essential both academically and clinically.
Anatomical and Physiological Differences
Children and infants differ from adults in several ways that affect CPR procedures:
Anatomical Differences
- Airway: More narrow, flexible, and susceptible to obstruction
- Tongue: Proportionally larger relative to the oral cavity
- Chest wall: More pliable with less musculature
- Ribs: More horizontal orientation
- Heart: Higher position in the chest
Physiological Differences
- Respiratory rate: Faster baseline respiratory rate
- Heart rate: Higher resting heart rate
- Metabolic rate: Higher oxygen consumption
- Blood volume: Lower total blood volume
- Respiratory reserves: Reduced
These differences are commonly tested in NEET previous year question papers and should be part of your last minute revision materials.
Causes of Cardiac Arrest: Children vs. Adults
Understanding the primary causes of cardiac arrest in pediatric patients helps inform appropriate response:
Primary Causes in Children
- Respiratory failure (most common)
- Drowning
- Severe asthma
- Choking/airway obstruction
- Trauma
- Severe infection (sepsis)
- Severe dehydration
Primary Causes in Adults
- Primary cardiac issues (most common)
- Coronary artery disease
- Arrhythmias
- Heart failure
This fundamental difference—that pediatric cardiac arrest usually begins with respiratory failure rather than a primary cardiac event—explains why the approach to pediatric resuscitation may emphasize airway and breathing slightly more than in adults. This concept is frequently covered in NEET books and certification courses.
Pediatric CPR: Ages 1 to Puberty
The CPR steps for children between 1 year and puberty follow this sequence:
1. Ensure Scene Safety
- Check for hazards before approaching
- Ensure your safety and the child's
2. Check Responsiveness
- Tap the shoulders gently
- Call the child's name loudly
- Look for any movement or response
3. Call for Help
- If alone with an unresponsive child:
- Perform 2 minutes of CPR first
- Then call emergency services and retrieve an AED
- If others are present:
- Direct someone to call emergency services and get an AED
4. Check Breathing and Pulse
- Look for absence of normal breathing or only gasping
- Check the carotid pulse (for a child) for no more than 10 seconds
- If no pulse or you're uncertain, begin CPR
5. Begin Chest Compressions
- Position the child on a firm, flat surface
- Place the heel of one or two hands (depending on child's size) on the lower half of the sternum
- Position your shoulders directly over your hands
6. Perform High-Quality Compressions
According to CPR compression rate guidelines:
- Compress at a rate of 100-120 compressions per minute
- Compress to a depth of at least one-third the depth of the chest (about 2 inches)
- Allow complete chest recoil after each compression
- Minimize interruptions in compressions
7. Provide Rescue Breaths
- After 30 compressions, deliver 2 rescue breaths (if trained)
- Open the airway using the head-tilt, chin-lift maneuver
- Each breath should last 1 second and make the chest visibly rise
- Maintain 30:2 compression-to-ventilation ratio for single rescuers
- For healthcare providers with advanced airway, provide continuous compressions with 1 breath every 2-3 seconds
This protocol is frequently included in NEET preparation books and certification exams.
Infant CPR: Under 1 Year of Age
The CPR procedure for infants has several important variations:
1-4. Initial Steps
- Follow the same initial assessment steps as for children
5. Begin Chest Compressions
- Position the infant on a firm, flat surface
- Draw an imaginary line between the nipples
- Place 2 fingers on the sternum just below this line
- OR encircle the chest with both hands and use both thumbs to compress (two-thumb technique, preferred for healthcare providers)
6. Perform High-Quality Compressions
- Compress at a rate of 100-120 compressions per minute
- Compress to a depth of at least one-third the depth of the chest (about 1.5 inches)
- Allow complete chest recoil after each compression
- Minimize interruptions in compressions
7. Provide Rescue Breaths
- After 30 compressions, deliver 2 rescue breaths
- Cover both the infant's mouth and nose with your mouth
- Use gentle breaths (just enough to make the chest rise)
- Maintain 30:2 compression-to-ventilation ratio for single rescuers
- For healthcare providers with advanced airway, provide continuous compressions with 1 breath every 2-3 seconds
Mastering these techniques is essential for NEET mock test preparation and clinical practice.
Compression Techniques: Age-Appropriate Approaches
The CPR equipment needed and techniques used vary by age:
Infant (Under 1 Year)
- Two-finger technique: For single rescuers, use two fingers to compress the chest
- Two-thumb encircling hands technique: For two rescuers, encircle the chest with both hands and use both thumbs to compress (preferred method for healthcare providers)
- Depth: Approximately 1.5 inches (4 cm) or one-third of chest depth
- Rate: 100-120 compressions per minute
- Ratio: 30:2 (single rescuer) or 15:2 (two healthcare providers)
Child (1 Year to Puberty)
- One or two hand technique: Use the heel of one hand for smaller children or two hands for larger children
- Depth: Approximately 2 inches (5 cm) or one-third of chest depth
- Rate: 100-120 compressions per minute
- Ratio: 30:2 (single rescuer) or 15:2 (two healthcare providers)
Proper hand positioning and technique are crucial and often featured in NEET tips and study materials.
Airway Management in Pediatric Resuscitation
Airway management has special considerations in pediatric resuscitation:
Head Position
- Infants: "Sniffing position" - neutral or slight extension
- Children: Slight extension of the neck
- Caution: Avoid overextension which can collapse the airway
Airway Maneuvers
- Head-tilt, chin-lift: Standard method
- Jaw thrust: Preferred in trauma cases to maintain cervical spine alignment
- Modified jaw thrust: May be used if trauma is suspected
Common Challenges
- Small airways: More easily obstructed
- Large tongues: Can block the airway
- Soft tissues: More compressible
- Anatomical differences: Higher larynx position
These airway considerations are essential knowledge for healthcare providers and feature prominently in CPR training materials.
CPR Ratios and Timing for Pediatric Patients
The CPR ratio guidelines for pediatric patients have subtle differences:
Single Rescuer
- 30:2 compression-to-ventilation ratio (same as adults)
- Complete 5 cycles before calling for help (if alone)
Two Healthcare Provider Team
- 15:2 compression-to-ventilation ratio (different from adult 30:2)
- Allows more frequent ventilation for respiratory-caused arrests
- Switch compressors every 2 minutes to prevent fatigue
With Advanced Airway
- Continuous compressions at 100-120 per minute
- 1 breath every 2-3 seconds (20-30 breaths per minute)
- No pausing of compressions for breaths
These ratios should be memorized using flashcard applications for NEET or similar study aids.
Foreign Body Airway Obstruction in Children
Choking is a common pediatric emergency that may require CPR:
Signs of Severe Airway Obstruction
- Unable to speak, cry, or make sounds
- Weak, ineffective cough
- No breathing or increased breathing difficulty
- Cyanosis (bluish discoloration)
- Loss of consciousness
Response for Responsive Child/Infant
- Child: Abdominal thrusts (Heimlich maneuver)
- Infant: 5 back blows followed by 5 chest thrusts
- Continue until object is expelled or child becomes unresponsive
Response for Unresponsive Child/Infant
- Begin CPR (start with compressions)
- Look in mouth before giving breaths (remove visible objects)
- Do not perform blind finger sweeps (risk of pushing object deeper)
This protocol is frequently tested in NEET exams and certification courses.
AED Use in Pediatric Resuscitation
AED use has specific considerations for pediatric patients:
General Guidelines
- Use pediatric pads/energy attenuator for children under 8 years if available
- If pediatric equipment is unavailable, use adult pads ensuring they don't overlap
- Place pads in anterior-posterior position for small children
- Follow the same general AED protocol as for adults
Energy Levels
- Automated pediatric doses: Typically 50-70 joules
- Manual defibrillation: 2-4 joules/kg initially, 4 joules/kg for subsequent shocks
Special Considerations
- Remove wet clothing if present
- Dry the chest before pad placement
- Ensure no one is touching the patient during analysis and shock
- Resume CPR immediately after shock delivery
These guidelines are covered in comprehensive CPR training courses and should be part of your NEET exam tips study plan.
Family Presence During Pediatric Resuscitation
Modern CPR guidelines acknowledge the importance of family presence during resuscitation:
Benefits of Family Presence
- Allows family to see all efforts were made
- Facilitates the grieving process
- May provide comfort to the child
- Helps family understand the severity of the situation
Recommended Approach
- Assign a dedicated staff member to support the family
- Prepare the family for what they will see and hear
- Allow the option to remain or leave
- Provide ongoing explanations of procedures
- Offer opportunities to touch or speak to the child when appropriate
This aspect of pediatric resuscitation represents evolving best practices in the field and may appear in forward-thinking NEET books and certification materials.
Post-Resuscitation Care for Pediatric Patients
After return of spontaneous circulation (ROSC), specialized care continues:
Immediate Interventions
- Secure the airway if not already done
- Optimize oxygenation and ventilation
- Monitor vital signs continuously
- Assess neurological status
- Maintain normal body temperature
- Avoid hyperthermia
- Consider therapeutic hypothermia in specific cases
Advanced Considerations
- Treat underlying causes
- Optimize hemodynamics
- Maintain glucose control
- Consider neuroprotective strategies
- Transfer to pediatric intensive care
Understanding the complete resuscitation cycle, including post-resuscitation care, is essential for comprehensive NEET preparation.
Conclusion: Preparing to Save Young Lives
Pediatric and infant CPR requires specific knowledge, skills, and practice. For healthcare professionals and those preparing for NEET MDS examinations, these specialized techniques represent critical competencies.
Remember that while the fundamentals of resuscitation remain constant, the anatomical and physiological differences in children demand these specialized approaches. By mastering pediatric and infant CPR, you prepare yourself not only for examinations but for those moments when a young life depends on your knowledge and skill.