Managing Complications in Tooth Extraction
Medi Study Go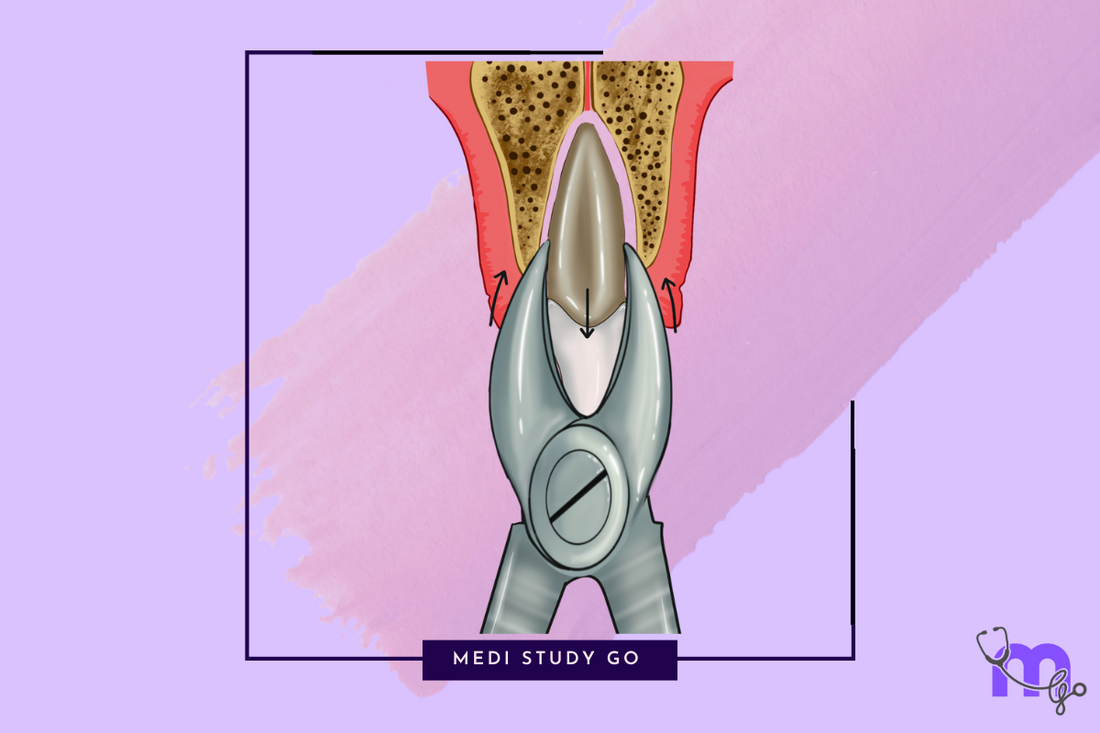
Related Resources
- Comprehensive Guide to Exodontia: Principles, Procedures, and Best Practices
- Complete Guide to Indications and Contraindications for Tooth Extraction
- Dental Extraction Instruments & Techniques: A Complete Guide
- Surgical Extraction Procedures: A Comprehensive Guide
- Post-Extraction Care and Healing
Introduction
Even with meticulous technique and proper precautions, complications can occur during or after tooth extraction procedures. The ability to recognize, prevent, and manage these complications is a critical skill for dental practitioners. This comprehensive guide explores common complications of tooth extraction, with detailed focus on dry socket (alveolar osteitis), one of the most frequent post-extraction complications.
Understanding these complications—their etiology, risk factors, prevention, and management—is not only essential for clinical practice but also a key area of knowledge for the NEET MDS examination.
Classification of Extraction Complications
Complications of tooth extraction can be classified based on their timing:
Intraoperative Complications
Occur during the extraction procedure:
- Fracture of tooth or root
- Damage to adjacent teeth
- Soft tissue injuries
- Fracture of alveolar bone
- Displacement of tooth or root fragments
- Nerve injuries
- Sinus exposure/perforation
- Mandibular fracture
- Temporomandibular joint injury
- Aspiration or ingestion of tooth/instruments
Postoperative Complications
Occur following the extraction procedure:
-
Immediate (within 24 hours):
- Hemorrhage
- Pain
- Swelling
- Ecchymosis
- Hematoma
-
Delayed (days to weeks):
- Alveolar osteitis (dry socket)
- Infection
- Prolonged trismus
- Delayed healing
- Neurosensory disturbances
-
Late (months to years):
- Residual root fragments
- Osteomyelitis
- Osteosclerosis
- Chronic pain
- Paresthesia
Intraoperative Complications and Management
1. Fracture of Tooth or Root
Causes:
- Excessive or improperly directed force
- Unfavorable root anatomy (dilacerated, bulbous, or hypercementosed roots)
- Ankylosis
- Weakened tooth structure due to caries or previous restorations
Prevention:
- Proper radiographic assessment
- Appropriate force application
- Sectioning of multi-rooted teeth when indicated
- Adequate socket expansion before elevation
Management:
- Visualize the fractured fragment
- Create adequate access if needed
- Use appropriate elevators (e.g., Cryer, Warwick James, root tip picks)
- Consider "window" technique for deeply positioned fragments
- Use gentle irrigation to improve visibility
- In some cases, small deeply positioned fragments with no pathology or symptoms may be left in place with patient consent and documentation
2. Damage to Adjacent Teeth
Causes:
- Improper fulcrum placement
- Excessive force
- Incorrect forceps application
- Poor visibility or access
Prevention:
- Careful assessment of adjacent teeth
- Proper instrument selection and application
- Controlled force application
- Protection of adjacent teeth during elevation
Management:
- Immediate assessment of damage
- Stabilization of loosened teeth (splinting if necessary)
- Restoration of damaged teeth as appropriate
- Documentation and follow-up
3. Soft Tissue Injuries
Causes:
- Slippage of instruments
- Improper retraction
- Sharp bone edges
- Excessive manipulation
Prevention:
- Proper retraction techniques
- Controlled instrument handling
- Adequate visibility
Management:
- Irrigation to clean wound
- Suturing when appropriate
- Pressure to control bleeding
- Post-operative instructions for care
4. Sinus Exposure/Perforation
Causes:
- Close proximity of maxillary posterior teeth roots to sinus
- Excessive apical pressure during extraction
- Aggressive curettage of sockets
Prevention:
- Proper radiographic assessment
- Controlled force application
- Careful socket debridement
Management:
- Assess size of communication
- For small perforations (<2mm):
- Blood clot formation and protection
- Avoid nose blowing, sneezing with closed mouth
- Prescribe decongestants and antibiotics
- For larger perforations:
- Consider flap advancement and closure
- Buccal fat pad graft for large perforations
- Refer to specialist if needed
5. Displacement of Tooth/Root Fragments
Common Displacement Spaces:
- Maxillary sinus
- Submandibular space
- Infratemporal fossa
- Lingual space
- Buccal space
Prevention:
- Proper radiographic assessment
- Controlled force application
- Use of gauze screens/throat packs for posterior teeth
- Adequate visibility and access
Management:
- Depends on location, size, and patient symptoms
- Radiographic localization
- Attempt retrieval if accessible
- Refer to specialist for complex displacements
- For maxillary sinus:
- Small asymptomatic fragments may be left with follow-up
- Larger fragments or symptomatic cases require surgical removal
Postoperative Complications and Management
1. Hemorrhage
Classification:
- Primary: Occurs during or immediately after extraction
- Reactionary: Within 24 hours of extraction
- Secondary: 2-10 days after extraction (often due to infection)
Causes:
- Local factors: Trauma to tissues, failure to follow post-op instructions
- Systemic factors: Coagulopathies, medications (anticoagulants), liver disease
- Vascular anomalies
Prevention:
- Thorough medical history
- INR testing for patients on anticoagulants
- Controlled surgical technique
- Adequate socket compression
- Hemostatic measures when indicated
Management:
- Identify source of bleeding
- Local measures:
- Pressure application with gauze (30 minutes)
- Removal of granulation tissue if present
- Suturing if needed
- Local hemostatic agents (gelfoam, surgicel, tranexamic acid)
- Control of systemic factors if present
- Hospitalization for severe uncontrolled cases
2. Alveolar Osteitis (Dry Socket)

Definition: Localized inflammation of the alveolar bone characterized by severe pain, partially or completely disintegrated blood clot, and exposed bone in the socket, typically developing 2-4 days after extraction.
Incidence:
- 3-25% following extraction of impacted mandibular third molars
- 1-4% in routine extractions
- More common in mandibular extractions than maxillary
Etiology and Pathogenesis:
Multiple theories exist, with the fibrinolysis theory (Birn's theory) being most accepted:
- Trauma and inflammation activate plasminogen
- Plasminogen converts to plasmin
- Plasmin causes lysis of the blood clot
- Dissolution of the protective blood clot exposes bone
- Bacterial action and tissue breakdown products produce pain
Risk Factors:
-
Local Factors:
- Traumatic extraction
- Excessive bone removal
- Infection at extraction site
- Poor oral hygiene
- Bone density (mandibular molars have denser bone)
- Inadequate blood supply
-
Systemic Factors:
- Smoking (increases risk by 2-5 times)
- Oral contraceptives (increased estrogen levels)
- Advanced age
- Female gender (especially during menstruation)
- Immunocompromised states
- History of previous dry socket
Clinical Features:
- Severe, throbbing pain developing 2-4 days after extraction
- Pain often radiates to ear, temporal region, or neck
- Partially or completely empty socket with exposed bone
- Foul odor and taste
- Absence of pus formation (distinguishes from infection)
- Regional lymphadenopathy may be present
Prevention:
-
Preoperative Measures:
- Oral hygiene instructions
- Prophylactic antibiotics in high-risk cases
- Antiseptic mouthwash (chlorhexidine)
- Smoking cessation advice
- Scheduling extraction during appropriate menstrual cycle phase for women
-
Intraoperative Measures:
- Atraumatic surgical technique
- Adequate irrigation
- Avoidance of excessive bone removal
- Application of local hemostatic agents
- Socket medicaments (PRF, collagen plugs)
-
Postoperative Measures:
- Detailed post-extraction instructions
- Avoid rinsing, spitting, smoking for 24 hours
- Avoid straw use or creating negative pressure
Management:
-
Palliative Care:
- Pain management (analgesics, NSAIDs)
- Local anesthesia if needed for severe pain
-
Local Treatment:
- Gentle irrigation with saline or antiseptic solution
- Debridement of necrotic debris
- Placement of medicated dressing:
- Zinc oxide eugenol paste
- Alvogyl (containing eugenol, iodoform, butamben)
- Ozone therapy in modern practice
- Socket packing with iodoform gauze soaked in eugenol
-
Follow-up Care:
- Dressing changes every 2-3 days as needed
- Continued analgesics until pain subsides
- Healing typically occurs within 7-14 days
- No specific intervention needed for socket healing
3. Post-Extraction Infection
Causes:
- Pre-existing infection
- Contamination during extraction
- Patient factors (immunocompromised status)
- Poor oral hygiene
- Retained root fragments or foreign bodies
Clinical Features:
- Persistent or increasing pain after 2-3 days
- Swelling and erythema
- Purulent discharge
- Fever and malaise
- Lymphadenopathy
- Limited mouth opening
Prevention:
- Appropriate antibiotic prophylaxis for high-risk cases
- Aseptic technique
- Complete removal of pathological tissue
- Thorough debridement and irrigation
Management:
- Drainage if fluctuant collection present
- Appropriate antibiotic therapy based on clinical presentation
- Analgesics for pain control
- Warm saline rinses
- Removal of any foreign body or sequestrum
- Referral if severe or spreading infection
4. Neurosensory Disturbances
Commonly Affected Nerves:
- Inferior alveolar nerve
- Lingual nerve
- Mental nerve
- Long buccal nerve
- Infraorbital nerve
Causes:
- Direct trauma during injection or extraction
- Compression from edema or hematoma
- Bone fragments impinging on nerve
- Chemical neuritis from local anesthetics
Classification:
- Neurapraxia: Temporary conduction block (most common)
- Axonotmesis: Disruption of axons with intact nerve sheath
- Neurotmesis: Complete transection of nerve (worst prognosis)
Prevention:
- Thorough radiographic assessment
- Knowledge of anatomical variations
- Careful surgical technique, especially for third molars
- Considered coronectomy for high-risk cases
Management:
-
Immediate Recognition and Documentation:
- Document area and nature of sensory alteration
- Reassure patient about typically transient nature
-
Follow-up Assessment:
- Regular neurosensory testing
- Monitoring for improvement
-
Treatment Based on Severity and Duration:
- Most cases resolve spontaneously within 6 months
- For persistent cases (>3 months):
- Medications: Corticosteroids, vitamin B complex
- Microneurosurgery for selected cases of persistent severe impairment
- Referral to specialist for advanced care
5. Trismus (Limited Mouth Opening)
Causes:
- Trauma to masticatory muscles
- Inflammation and edema
- Hematoma formation
- Excessive use of inferior alveolar nerve block
- Infection spreading to masticatory spaces
Prevention:
- Proper injection technique
- Gentle tissue manipulation
- Controlled surgical trauma
- Appropriate postoperative instructions
Management:
- Moist heat application
- Anti-inflammatory medications
- Muscle relaxants when indicated
- Progressive jaw opening exercises
- Physical therapy for persistent cases
- Address underlying cause (infection, etc.)
Special Considerations: Surgical Complications
1. Oro-antral Communication
Risk Factors:
- Maxillary molar extractions (particularly first molar)
- Pneumatized sinuses
- Roots projecting into sinus
- Periapical pathology extending to sinus floor
Diagnosis:
- Bubbling of blood in socket with respiration
- Air passing from nose to mouth
- Valsalva test (nose blowing with nostrils pinched)
- Nasal escape during speech
Management Based on Size:
-
Small communications (<2mm):
- Blood clot preservation
- Avoid pressure changes (no nose blowing, sneezing, smoking)
- Antibiotics and decongestants
- Self-resolving with proper care
-
Medium communications (2-6mm):
- Buccal advancement flap
- Palatal rotation flap
- Buccal fat pad graft
-
Large communications (>6mm):
- Combined approaches
- Referral to oral-maxillofacial surgeon
2. Displacement of Teeth into Anatomic Spaces
Common Displacement Locations:
- Maxillary sinus (maxillary molars)
- Infratemporal fossa (maxillary third molars)
- Submandibular space (mandibular molars)
- Lateral pharyngeal space (mandibular third molars)
Management Principles:
- Radiographic localization (panoramic, CBCT)
- Attempt immediate retrieval if visible
- If not immediately retrievable:
- For maxillary sinus: Caldwell-Luc approach or endoscopic retrieval
- For infratemporal fossa: Often deferred unless symptomatic
- For tissue spaces: Surgical access and exploration
- Antibiotics to prevent infection
- Referral to specialist for complex cases
3. Mandibular Fracture
Risk Factors:
- Atrophic mandible
- Large cystic lesions
- Impacted third molars in elderly
- Excessive force during extraction
- Pre-existing pathology weakening bone
Prevention:
- Radiographic assessment
- Sectioning teeth when indicated
- Controlled force application
- Consider referral for high-risk cases
Management:
- Immediate recognition
- Stabilization
- Referral for definitive management (typically ORIF)
- Antibiotics and soft diet during healing
Complications Specific to Medically Compromised Patients
1. Bleeding Disorders
Complications:
- Prolonged or excessive bleeding
- Hematoma formation
- Delayed healing
Management:
- Consultation with hematologist
- Local hemostatic measures
- Modification of anticoagulant therapy when appropriate
- Consider admission for severe cases
2. Cardiovascular Conditions
Complications:
- Hypertensive crisis
- Angina episodes
- Arrhythmias
- Myocardial infarction
Management:
- Stress reduction protocols
- Short appointments
- Vital sign monitoring
- Emergency medications available
- Immediate medical referral for serious events
3. Diabetes Mellitus
Complications:
- Delayed healing
- Increased infection risk
- Hypoglycemic episodes
Management:
- Ensure glycemic control
- Prophylactic antibiotics for poorly controlled cases
- Monitor for hypoglycemia
- Extended follow-up for wound healing
Prevention of Extraction Complications
1. Proper Patient Assessment
- Thorough medical history
- Comprehensive clinical examination
- Appropriate radiographic evaluation
- Risk assessment and management
2. Technique Considerations
- Appropriate instrument selection
- Controlled force application
- Adequate visibility and access
- Proper surgical technique
3. Patient Education
- Clear pre-operative instructions
- Detailed post-operative instructions
- Warning signs requiring return
- Scheduled follow-up appointments
4. Operator Factors
- Knowledge of anatomy
- Recognition of limitations
- Willingness to refer complex cases
- Continuous skill development
Documentation and Medical-Legal Considerations
Proper documentation is essential when complications occur:
-
Preoperative Documentation:
- Informed consent with specific risks discussed
- Preoperative condition and radiographs
- Treatment plan and alternatives discussed
-
Intraoperative Documentation:
- Technique used
- Any complications encountered
- Management steps taken
- Immediate postoperative status
-
Postoperative Documentation:
- Instructions provided
- Follow-up appointments
- Complication management
- Patient compliance with instructions
Conclusion
Complications are an inherent risk in tooth extraction procedures. The ability to anticipate, prevent, recognize, and manage these complications is essential for optimal patient care. Through thorough knowledge, careful technique, and appropriate management protocols, many complications can be prevented or minimized.
For dental students preparing for the NEET MDS exam, understanding these complications—particularly dry socket (alveolar osteitis) and other common postoperative issues—is crucial for both theoretical knowledge and clinical practice.
Remember that prompt recognition and appropriate management of complications not only improves patient outcomes but also strengthens the practitioner-patient relationship through demonstrated competence and care.