Major Connectors in Removable Partial Dentures: A Comprehensive Guide
Medi Study Go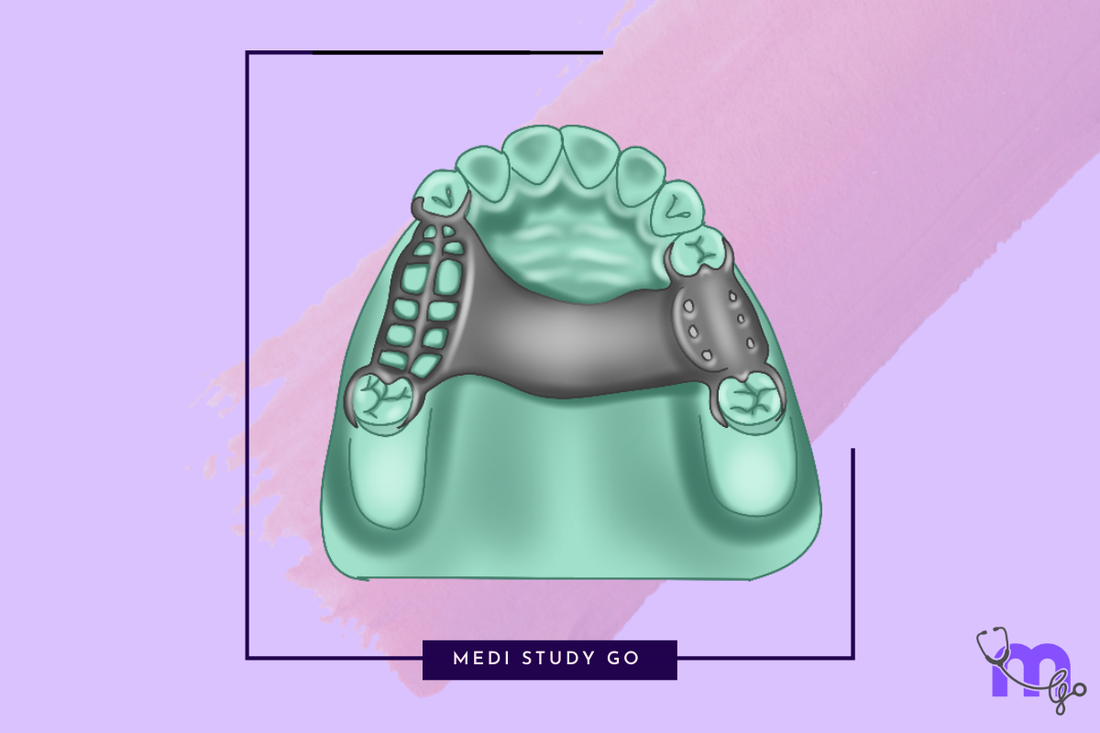
Related Resources:
- Maxillary Major Connectors: Types, Indications, and Selection Criteria
- Mandibular Major Connectors: Complete Design Guide
- Major Connectors Classification Systems: An Evidence-Based Approach
- Major and Minor Connectors: Understanding Their Interrelationship
- Major Connectors for Kennedy Class Situations: Clinical Guidelines
Introduction to Major Connectors

A major connector is the fundamental component of any removable partial denture (RPD) that unites all parts of the prosthesis across the arch. This critical element connects components on one side of the dental arch to those on the opposite side, providing essential rigidity and stability to the entire prosthetic structure.
For dental students preparing for the NEET examination, understanding major connectors is crucial not only for answering NEET previous year question papers but also for developing clinical competence. Major connectors serve multiple vital functions that directly impact the success and longevity of partial dentures in clinical practice.
Essential Functions of Major Connectors:
- Unifying all components of the partial denture
- Distributing forces across the entire dental arch
- Providing rigidity to resist deformation
- Supporting denture bases
- Contributing to indirect retention where indicated
- Protecting underlying tissues
As you review your NEET preparation books and NEET mock tests, you'll find that questions about major connectors frequently appear, making this knowledge indispensable for exam success.
Basic Requirements for Major Connectors
Regardless of whether they're designed for the maxillary or mandibular arch, all major connectors must fulfill certain fundamental requirements:
Rigidity
Major connectors must resist deformation under functional loads. Even minimal flexing can lead to:
- Increased stress on abutment teeth
- Patient discomfort
- Compromised retention
- Potential tissue damage
Proper Tissue Coverage
The connector must be designed to optimize support without causing:
- Patient discomfort
- Tissue irritation
- Interference with normal function
- Phonetic issues
Patient Compatibility
The best major connector design balances technical requirements with patient comfort by:
- Minimizing bulk where possible
- Avoiding interference with tongue movement and speech
- Working harmoniously with existing oral anatomy
For successful last minute revision before exams, remember that every major connector must balance these sometimes competing demands based on individual patient circumstances.
Classification of Major Connectors
Major connectors are primarily classified based on the arch they serve, with each category having distinct design considerations due to anatomical differences.
Primary Classification:
- Maxillary Major Connectors - For the upper arch
- Mandibular Major Connectors - For the lower arch
Within each category, various designs have been developed to address specific clinical situations. The selection process involves considering multiple factors, including:
- Kennedy classification of partial edentulism
- Location and number of remaining teeth
- Condition of supporting tissues
- Anatomical considerations (e.g., palatal vault shape, tori)
- Patient factors (comfort, aesthetics, speech)
- Biomechanical requirements
Using flashcard techniques for study to memorize these classifications and their indications can be an effective NEET revision tool.
Maxillary Major Connectors Overview
Maxillary major connectors are designed to utilize the palatal area for support and stability. Their design must balance coverage of the hard palate with patient comfort and function.
Common Types of Maxillary Major Connectors:
1. Palatal Strap
- Design: Wide band of metal with thin cross-sectional dimension (minimum 8mm anteroposterior dimension)
- Indications: Kennedy Class II (unilateral distal extension) and Class III situations
- Advantages: Great resistance to bending, minimal tongue interference, distributed stress
- Limitations: Not suitable for Kennedy Class I (bilateral distal extension)
2. Palatal Bar
- Design: Narrow, half-oval shape with thickest point at center
- Indications: Interim applications, short-span Class III situations
- Advantages: Simple design with moderate tissue coverage
- Disadvantages: Less comfortable due to bulk needed for rigidity
3. Horseshoe Bar
- Design: Thin band of metal running along lingual surfaces of remaining teeth
- Indications: Replacing anterior teeth without extensive palatal coverage, presence of torus palatinus
- Advantages: Reasonably strong, can avoid bony prominences
- Disadvantages: Less rigid, tendency to flex or deform
4. Anteroposterior Palatal Strap
- Design: Combination of anterior and posterior straps connected longitudinally
- Indications: Accommodation of torus palatinus
- Advantages: Rigid with minimum tissue coverage, resistant to deformation
- Disadvantages: Often uncomfortable, limited palatal support
5. Complete Palate
- Design: Maximum palatal coverage
- Indications: When all posterior teeth need replacement, compromised periodontal support
- Advantages: Extremely rigid, comfortable, good thermal conductivity
- Disadvantages: Possible tissue reactions, occasional speech issues
Mandibular Major Connectors Overview
Mandibular connectors face different challenges compared to maxillary designs due to the arc-shaped mandible and the presence of movable tissues in the floor of the mouth.
Common Types of Mandibular Major Connectors:
1. Lingual Bar
- Design: Half-pear in cross-section (minimum 5mm height)
- Indications: Most common design when sufficient vertical space exists
- Advantages: Simple design, minimal tissue contact, decreased plaque accumulation
- Limitations: Requires sufficient space between gingiva and floor of mouth
2. Lingual Plate
- Design: Thin metal piece with scalloped appearance extending onto lingual tooth surfaces
- Indications: Insufficient vertical space, high muscle attachments, periodontally compromised teeth
- Advantages: Exceptional rigidity, minimal tongue interference
- Disadvantages: Potential enamel decalcification, tissue irritation
3. Sublingual Bar
- Design: Modification of lingual bar placed inferiorly and posteriorly
- Indications: Insufficient floor height, anterior lingual undercuts, interfering tori
- Limitations: Contraindicated with high lingual frenum or elevated floor of mouth
4. Double Lingual Plate
- Design: Combines features of lingual bar and plate with two connected components
- Indications: When contact with mandibular anterior teeth is necessary with open embrasures
- Advantages: Provides indirect retention, promotes saliva flow
- Disadvantages: Difficult adaptation with crowded anteriors, possible tongue irritation
5. Labial Bar/Swing Lock
- Design: Bar extending across facial mucosa, sometimes with hinge mechanism
- Indications: Missing key abutments, unfavorable contours, questionable prognosis teeth
- Advantages: Alternative when lingual connectors contraindicated
- Disadvantages: Poor esthetics, potential for distal rotation of abutments
Major Connectors and Kennedy Classification
The Kennedy classification system for partially edentulous arches significantly influences major connector selection. Understanding this relationship is essential for NEET exam tips and clinical practice.
Kennedy Class I (Bilateral Posterior Edentulous Areas)
- Maxillary: Complete palate or anteroposterior palatal strap recommended
- Mandibular: Lingual bar or lingual plate preferred
- Rationale: Maximum support and rigidity needed for bilateral distal extension
Kennedy Class II (Unilateral Posterior Edentulous Area)
- Maxillary: Palatal strap often suitable
- Mandibular: Lingual bar commonly used
- Rationale: Balanced support needed with consideration for the remaining dentition
Kennedy Class III (Bounded Edentulous Area)
- Maxillary: Various options including palatal bar or strap
- Mandibular: Lingual bar typically sufficient
- Rationale: Tooth-supported design allows for more options
Kennedy Class IV (Anterior Edentulous Area)
- Maxillary: Horseshoe design may be considered if appropriate
- Mandibular: Lingual plate often beneficial
- Rationale: Anterior replacement requires consideration of esthetics and support.
Biomechanical Considerations
Proper major connector design requires understanding the biomechanical principles that govern RPD function. These principles directly influence the success of the prosthesis and patient satisfaction.
Stress Distribution
Major connectors must properly distribute functional forces to:
- Prevent localized stress concentration
- Protect abutment teeth from excessive forces
- Maintain tissue health beneath the prosthesis
- Ensure longevity of the restoration
Cross-Sectional Design
The dimensions and shape of the connector dramatically affect rigidity:
- Increased width improves rigidity but may compromise comfort
- Thin cross-sections require wider designs for equivalent rigidity
- Half-pear shapes provide optimal rigidity-to-bulk ratio for mandibular connectors
Border Considerations
Properly designed borders are essential for patient acceptance:
- All borders should be smooth and rounded
- Placement should avoid frenum attachments and mobile tissues
- Junctions between connectors and other components should be gradual
Understanding these biomechanical principles is crucial for NEET MDS candidates and appears frequently in previous year question papers.
Clinical Decision-Making Process
Selecting the appropriate major connector involves a systematic approach that considers multiple factors:
Patient Assessment
- Anatomical Evaluation: Palatal vault form, presence of tori, frenal attachments
- Periodontal Status: Health of remaining dentition
- Tissue Resilience: Quality and support capability of edentulous areas
- Functional Considerations: Speech patterns, tongue size and mobility
Special Considerations
- Gag Reflex: May contraindicate extensive palatal coverage
- Patient Expectations: Comfort vs. optimal biomechanical design
- Previous Prosthetic Experience: Adaptation to similar designs
- Maintenance Capability: Patient's ability to maintain oral hygiene
Diagnostic Procedures
- Diagnostic Casts: Analysis of undercuts and topographical features
- Framework Design Mapping: Planning path of insertion and connector boundaries
- Mock-ups: When necessary to verify comfort and speech
Using flashcard applications for NEET to review these decision-making factors can enhance retention and clinical application of this knowledge.
Common Problems and Solutions
Understanding common issues with major connectors helps in both exam preparation and clinical problem-solving.
Design-Related Issues
- Insufficient Rigidity: Results in movement, discomfort, and potential tissue damage Solution: Increase connector width or thickness while maintaining comfortable contours
- Excessive Bulk: Causes patient discomfort and speech problems Solution: Redesign using alternative connector type or modify cross-sectional shape
- Improper Border Placement: Leads to tissue impingement and irritation Solution: Respect anatomical landmarks and provide relief where necessary
Clinical Complications
- Tissue Irritation: Often seen with improperly finished or designed connectors Solution: Smooth all borders and ensure proper relief of vulnerable tissues
- Speech Alterations: Particularly with maxillary connectors that interfere with tongue movement Solution: Modify connector design or position to minimize phonetic interference
- Poor Patient Acceptance: Usually related to comfort or esthetic concerns Solution: Consider patient preferences in the initial design phase while maintaining biomechanical principles
Advancements in Major Connector Design
Modern prosthodontics continues to evolve, bringing innovations to major connector design and fabrication.
Digital Design and Fabrication
- CAD/CAM technology allows precise designing and milling
- Virtual try-in before fabrication
- Improved fit and adaptation
Material Innovations
- High-strength metal alloys with improved properties
- Metal-free alternatives for specific situations
- Hybrid designs incorporating multiple materials
Biomimetic Approaches
- Designs that better mimic natural oral function
- Stress-breaking mechanisms
- Tissue-friendly materials and finishes
These advancements continue to improve outcomes and are increasingly featured in NEET books and examination content.
NEET MDS Examination Tips for Major Connectors
For students preparing for NEET MDS examinations, major connectors represent an important topic that frequently appears in various question formats.
Common Question Patterns
- Classification and identification of major connector types
- Indications and contraindications for specific designs
- Dimensions and critical design features
- Problem-solving scenarios based on case presentations
Study Approaches
- Create comparison charts of different connector types
- Memorize key dimensions and design specifications
- Practice drawing major connector designs
- Review NEET PYQs (previous year questions) focusing on major connectors
Critical Concepts to Master
- Differences between maxillary and mandibular connector requirements
- Relationship between Kennedy classification and connector selection
- Biomechanical principles governing connector design
- Clinical decision-making process
Using last minute revision tools like flowcharts and summary tables can help consolidate this information before your exam.
Conclusion
Major connectors are foundational elements in removable partial denture design that influence the biomechanical performance, patient comfort, and long-term success of the prosthesis. Understanding their classification, design principles, and selection criteria is essential for both academic success in examinations like NEET MDS and clinical excellence in prosthodontic practice.
From the basic palatal strap to the complex swing lock design, each major connector type offers specific advantages and limitations that must be carefully weighed against patient needs and clinical realities. The systematic approach to major connector selection presented in this guide provides a framework for both examination preparation and clinical decision-making.
