Major Connectors for Kennedy Class Situations: Clinical Guidelines
Medi Study Go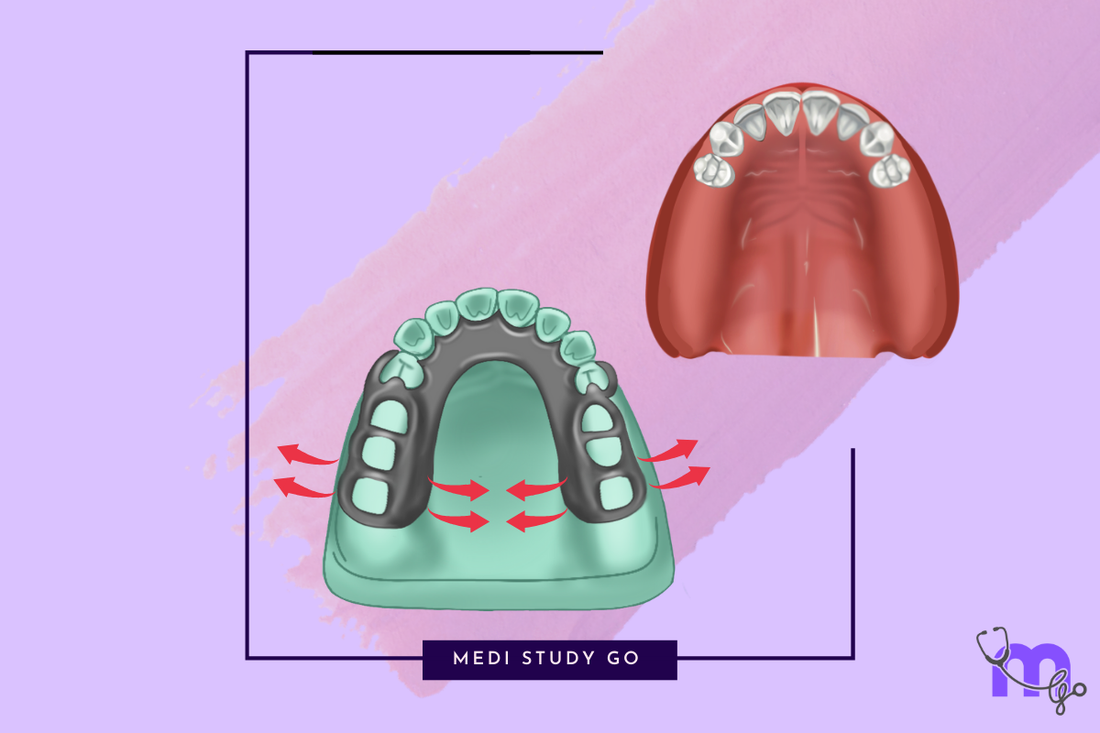
Related Resources:
- Major Connectors in Removable Partial Dentures: A Comprehensive Guide
- Maxillary Major Connectors: Types, Indications, and Selection Criteria
- Mandibular Major Connectors: Complete Design Guide
- Major Connectors Classification Systems: An Evidence-Based Approach
- Major and Minor Connectors: Understanding Their Interrelationship
Introduction to Kennedy Classification and Major Connectors
The Kennedy classification system for partially edentulous arches provides a standardized approach to categorizing clinical situations that directly influences major connector selection. Understanding the relationship between these classifications and appropriate connector choices is essential for creating biomechanically sound removable partial dentures (RPDs).
For dental students preparing for the NEET MDS examination, mastering this relationship is crucial, as questions connecting Kennedy classifications with major connector selection frequently appear in NEET previous year question papers and represent a core competency in prosthodontic knowledge.
Kennedy Classification Review

Before exploring specific connector recommendations, let's briefly review the Kennedy classification system that forms the foundation for these clinical decisions:
Kennedy Class I
Bilateral posterior edentulous areas (free-end saddles)
- Both posterior edentulous areas extend beyond the natural dentition
- No posterior abutment teeth present
Kennedy Class II
- Unilateral posterior edentulous area (free-end saddle)
- The edentulous area extends beyond the natural dentition on one side only
- No posterior abutment tooth present on the affected side
Kennedy Class III
- Unilateral posterior edentulous area with natural teeth remaining both anterior and posterior to the space
- Bounded saddle with abutment teeth present on both ends
Kennedy Class IV
- Single anterior edentulous area crossing the midline
- Anterior to the remaining natural teeth
Major Connector Selection by Kennedy Classification
The appropriate major connector choice depends on several factors including:
- Kennedy classification
- Arch form and tissue undercuts
- Periodontal status of remaining teeth
- Presence of tori or exostoses
- Need for indirect retention
- Patient comfort and esthetic concerns
Let's examine the ideal major connector choices for each Kennedy classification:
Kennedy Class I: Major Connector Recommendations
For Maxillary Arch:
-
Horseshoe-shaped palatal connector
- Indicated for patients with severe gag reflex
- Must be rigid and have adequate width (8-10mm minimum)
- Contraindicated in cases with poor periodontal support
-
Complete palatal plate
- Most commonly recommended
- Provides maximum cross-arch stabilization
- Excellent distribution of stress
- Particularly indicated when indirect retention is critical
-
Anteroposterior palatal strap
- Combines anterior and posterior palatal straps
- Good rigidity while conserving palatal coverage
- Better patient acceptance than complete plate
For Mandibular Arch:
-
Lingual bar
- Most common choice when adequate lingual vestibule depth exists (7mm+)
- Simple design with minimal tissue coverage
- Must be positioned at least 4mm from gingival margin
-
Lingual plate
- Indicated when inadequate vestibule depth exists
- Provides excellent cross-arch stabilization
- Indicated for periodontally compromised teeth requiring splinting
Kennedy Class II: Major Connector Recommendations
For Maxillary Arch:
-
Single palatal strap
- Often adequate due to unilateral stress pattern
- Width minimum of 8mm for adequate rigidity
- Most comfortable for patients
-
U-shaped palatal connector
- Provides additional rigidity
- Indicated when more stabilization is needed
For Mandibular Arch:
-
Lingual bar
- Generally sufficient for most Class II cases
- Minimizes interference with tongue movement
- Must have adequate connector height (at least 5mm)
-
Lingual plate
- For cases with periodontal compromise or inadequate vestibule depth
- Provides additional indirect retention
Kennedy Class III: Major Connector Recommendations
For Maxillary Arch:
-
Single palatal strap
- Most commonly recommended
- Minimizes palatal coverage
- Width of 8-10mm for adequate rigidity
-
Ring palatal connector
- Alternative for certain bounded saddle configurations
- Provides excellent cross-arch stabilization
For Mandibular Arch:
-
Lingual bar
- Ideal for most Class III cases
- Simple design with excellent patient acceptance
- Minimum of 5mm height for adequate rigidity
-
Sublingual bar
- Alternative when lingual tori are present
- Follows contour of lingual alveolar ridge
Kennedy Class IV: Major Connector Recommendations
For Maxillary Arch:
-
Anteroposterior palatal strap
- Optimal for anterior replacement
- Provides support for anterior teeth
- Better rigidity than single strap
-
Complete palatal plate
- Indicated when extensive anterior replacement is needed
- Provides maximum support and indirect retention
For Mandibular Arch:
-
Lingual bar with labial bar
- Combination required for anterior tooth replacement
- Labial bar provides support for anterior teeth
-
Lingual plate with labial bar
- When periodontal support is compromised
- Maximum stabilization for anterior replacement
Clinical Considerations in Major Connector Selection
-
Biomechanical Considerations
- Class I and II (free-end saddles) require more rigid connectors to resist rotation
- Class III typically requires less extensive connectors due to bounded support
- Class IV requires connectors that provide anterior stabilization
-
Anatomical Limitations
- Presence of tori may contraindicate certain connectors
- Shallow vestibules influence mandibular connector selection
- Pronounced palatal vault affects maxillary connector design
-
Indirect Retention Requirements
- More critical in Kennedy Class I and II cases
- Major connector design must complement indirect retainer placement
- Particularly important for distal extension bases
-
Patient-Related Factors
- Gag reflex sensitivity influences maxillary connector coverage
- Speech considerations, especially with maxillary anterior-posterior connectors
- Esthetic concerns with visible connectors
NEET MDS Examination Focus Areas
For NEET MDS preparation, focus on these high-yield topics regarding major connectors:
-
Key dimensional requirements:
- Minimum width for palatal straps (8-10mm)
- Minimum thickness for mandibular lingual bar (4-5mm height, 2mm thickness)
- Distance from gingival margin (minimum 4mm)
-
Contraindications for specific connectors:
- When lingual bar is contraindicated
- When horseshoe connector is inappropriate
- Modifications needed for anatomical variations
-
Stress distribution principles:
- How connector design influences force distribution
- Relationship between major connector rigidity and RPD success
- Signs of inadequate connector rigidity
-
Function-specific selection criteria:
- How free-end saddles influence connector choice
- Indirect retention requirements by Kennedy class
- Cross-arch stabilization principles
Clinical Case Scenarios
For effective exam preparation, practice with these common NEET MDS scenario-based questions:
- A 55-year-old patient presents with a Kennedy Class I maxillary arch and pronounced gag reflex. Which major connector would be most appropriate?
- A patient with mandibular Kennedy Class III modification 1 has significant lingual tori. What major connector would you recommend?
- A maxillary Kennedy Class IV case requires replacement of four anterior teeth with moderate periodontal compromise of remaining teeth. Select the most appropriate major connector.
- A patient with mandibular Kennedy Class II has shallow lingual vestibules measuring 5mm. Which major connector design is indicated?
Conclusion
The selection of appropriate major connectors based on Kennedy classification represents a critical decision point in removable partial denture design. By systematically evaluating the biomechanical requirements of each classification alongside patient-specific factors, clinicians can create prostheses that optimize function, comfort, and longevity.
For NEET MDS examination success, focus on understanding not just the "what" but the "why" behind connector selection—the principles that guide these choices across various clinical scenarios will form the foundation for both examination excellence and clinical competence.