Advanced Composite Materials in Dentistry: Innovations and Future Directions
Medi Study Go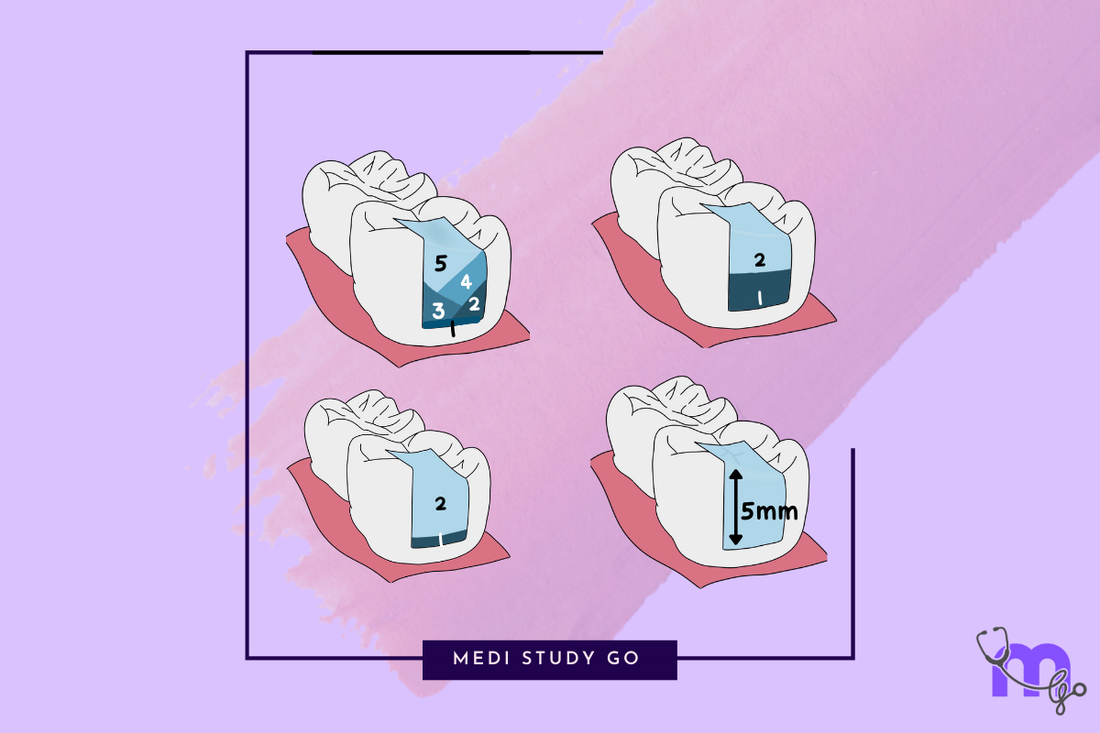
The landscape of dental composites continues to evolve rapidly, with exciting innovations addressing traditional limitations and opening new possibilities for clinical applications. For NEET MDS aspirants and dental professionals, understanding these advanced materials is essential for both examination preparation and future clinical practice.
Explore our complete dental composites series:
This comprehensive guide explores cutting-edge developments in composites and advanced materials, highlighting recent innovations, emerging technologies, and future directions in the field.
Bulk-Fill Composites: Evolution and Capabilities

Bulk-fill composites represent one of the most significant recent advancements in restorative dentistry, addressing the technique sensitivity and time requirements of traditional incremental placement.
Technology Behind Bulk-Fill Materials
Key Innovations:
- Enhanced Translucency: Allows deeper light penetration
- Modified Photoinitiator Systems: More efficient polymerization
- Polymerization Modulators: Reduced shrinkage stress
- Rheological Modifiers: Improved adaptation to cavity walls
- Novel Monomers: Lower volumetric shrinkage
Clinical Advantages:
- Placement in 4-5mm increments
- Reduced chair time
- Simplified technique
- Potentially fewer voids between layers
- Decreased technique sensitivity
Types of Bulk-Fill Composites
Flowable Bulk-Fill Composites
Characteristics:
- Lower viscosity for adaptation
- Self-leveling properties
- Generally requires conventional composite cap layer
- Excellent adaptation to irregular cavity surfaces
Clinical Applications:
- Deep box preparations in Class II restorations
- Base layer in sandwich technique
- Core build-ups under crowns
- Complex cavity geometries
Examples:
- SDR Flow+ (Dentsply Sirona)
- Filtek Bulk Fill Flowable (3M ESPE)
- Venus Bulk Fill (Kulzer)
High-Viscosity Bulk-Fill Composites
Characteristics:
- Packable consistency
- No capping layer required
- Higher filler content than flowable versions
- Improved wear resistance
Clinical Applications:
- Complete posterior restorations
- One-step bulk restorations
- Time-efficient procedures
- Pediatric restorations
Examples:
- Tetric EvoCeram Bulk Fill (Ivoclar Vivadent)
- Filtek One Bulk Fill (3M ESPE)
- SonicFill (Kerr)
Clinical Performance and Limitations
Current Evidence:
- Comparable physical properties to conventional composites
- Acceptable clinical performance in medium-term studies
- Reduced incidence of post-operative sensitivity
- Similar marginal adaptation to incremental placement
Remaining Challenges:
- Limited long-term clinical data
- Potential concerns about degree of conversion in deep portions
- Curing light intensity requirements
- Case selection considerations
Nanocomposites: The Microscopic Revolution
Nanotechnology has transformed dental composites by enabling manipulation of materials at the nanoscale (1-100 nm), resulting in enhanced properties.
Nanofill Technology
Fundamental Principles:
- Particles ranging from 5-100 nm
- Dramatically increased surface area to volume ratio
- Primary nanoparticles and nanoclusters
- Optimized filler loading despite small particle size
Material Properties:
- Exceptional polishability
- Superior gloss retention
- Improved wear resistance
- Enhanced optical properties
- Maintained mechanical strength
Clinical Applications:
- High-end anterior esthetics
- Areas requiring excellent polish retention
- Universal applications combining strength and esthetics
- Minimally invasive restorations
Examples:
- Filtek Supreme Ultra (3M ESPE)
- Estelite Sigma Quick (Tokuyama)
- Herculite Ultra (Kerr)
Nanohybrid Technology
Composition:
- Combination of nanoparticles with larger particles
- Integration of nano and conventional technologies
- Optimized filler distribution
- Balance between nanoparticle benefits and traditional strength
Material Properties:
- Balanced strength and esthetics
- Better handling than pure nanofills
- Good polishability
- Excellent wear parameters
- Versatile clinical performance
Clinical Applications:
- Universal restorative material
- High-load bearing areas
- Esthetic anterior applications
- Deep posterior restorations
Examples:
- Tetric EvoCeram (Ivoclar Vivadent)
- Ceram.X (Dentsply Sirona)
- Premise (Kerr)
Future Directions in Nanocomposite Technology
Emerging Developments:
- Self-assembling nanostructures
- Biomimetic nano-layered composites
- Quantum dot incorporations for enhanced properties
- Surface nanostructuring for improved integration
- Interactive nanomaterials with adaptive properties
Potential Benefits:
- Closer replication of natural tooth structure
- "Smart" materials with responsive properties
- Enhanced integration with biological systems
- Improved longevity through self-healing capabilities
- Reduced polymerization shrinkage
Smart Composites: Beyond Passive Restorations
A new generation of "smart" composites is emerging with capabilities to interact with their environment and respond to changing conditions.
Remineralizing Composites
Mechanism of Action:
- Release of calcium and phosphate ions
- Amorphous calcium phosphate (ACP) technology
- Bioactive glass incorporation
- Reservoir effect with ion rechargeability
- pH-responsive release systems
Clinical Benefits:
- Potential caries prevention around restorations
- Remineralization of adjacent demineralized tissue
- Self-repair of marginal defects
- Extended restoration longevity
- Reduced secondary caries risk
Examples:
- Beautifil II (Shofu Dental) - Giomer technology
- Activa BioActive (Pulpdent) - Bioactive ionic resin
- Cention N (Ivoclar Vivadent) - Alkaline filler technology
Self-Healing Composites
Technological Approaches:
- Microcapsule healing systems
- Hollow fiber delivery
- Microvascular networks
- Shape memory polymers
- Dynamic chemical bonds
Potential Advantages:
- Automatic repair of microcracks
- Extended material lifespan
- Reduced replacement frequency
- Sealing of marginal gaps
- Recovery from wear and fatigue
Research Status:
- Primarily in developmental stages
- Laboratory proof-of-concept demonstrations
- Emerging clinical prototypes
- Challenges in long-term stability
- Promising medium-term results
Antibacterial Composites
Mechanism of Action:
- Quaternary ammonium methacrylate incorporation
- Silver nanoparticle technology
- Zinc oxide nanoparticles
- Photocatalytic particles
- Controlled-release antimicrobial agents
Clinical Benefits:
- Reduction in biofilm formation
- Decreased risk of secondary caries
- Extended restoration longevity
- Potential benefits for high-caries risk patients
- Protection of cavity margins
Examples and Development Status:
- ACTIVA BioACTIVE (Pulpdent)
- Experimental formulations in clinical trials
- Increasing commercial availability
- Growing evidence base for efficacy
- Integration with existing composite technology
Low-Shrinkage Composites: Addressing a Fundamental Challenge
Polymerization shrinkage remains one of the primary limitations of composite materials. Advanced technologies are now addressing this challenge through innovative approaches.
Silorane-Based Composites
Technology:
- Ring-opening polymerization chemistry
- Siloxane and oxirane molecular components
- Cationic polymerization mechanism
- Fundamentally different from methacrylate systems
Advantages:
- Significantly reduced volumetric shrinkage (<1%)
- Decreased polymerization stress
- Reduced cuspal deflection
- Improved marginal integrity
- Less post-operative sensitivity
Clinical Considerations:
- Requires dedicated adhesive system
- Different handling characteristics
- Slower curing reaction
- Limited shade range
- Transitioning to newer technology platforms
Ormocer (Organically Modified Ceramic) Technology
Composition:
- Inorganic-organic copolymers
- Three-dimensionally cross-linked ceramics
- Pre-polymerized larger molecules
- Modified siloxane backbone
- Reduced concentration of reactive groups
Advantages:
- Lower polymerization shrinkage
- Reduced shrinkage stress
- Improved biocompatibility
- High surface hardness
- Good wear resistance
Clinical Applications:
- Universal restorative materials
- Biocompatibility-focused applications
- Reduced shrinkage stress situations
- High-wear environments
- Patients with biocompatibility concerns
Examples:
- Admira Fusion (VOCO)
- Ceram.X Spectra ST (Dentsply Sirona)
- Grandio (VOCO)
Stress-Decreasing Resin Technology
Approaches:
- Addition of polymerization stress relievers
- Incorporation of elastic monomers
- Stress-absorbing microdomains
- Delayed gelation strategies
- Thixotropic modifiers for flow during early polymerization
Benefits:
- Reduced polymerization stress without changing chemistry
- Compatible with conventional bonding systems
- Familiar handling characteristics
- Reduced gap formation
- Less cuspal flexure
Examples:
- SDR Flow+ (Dentsply Sirona)
- Filtek One Bulk Fill (3M ESPE)
- Tetric EvoCeram Bulk Fill (Ivoclar Vivadent)
Fiber-Reinforced Composites: Enhanced Structural Integrity
The incorporation of fibers into composite materials has opened new possibilities for extended applications requiring enhanced mechanical properties.
Types of Reinforcing Fibers
Glass Fibers:
- Most commonly used in dentistry
- Excellent strength-to-weight ratio
- Good esthetic integration
- Compatible with resin matrices
- Available in various configurations
Polyethylene Fibers:
- Ultrahigh molecular weight
- Exceptional toughness
- Virtually invisible in resin matrix
- Excellent handling characteristics
- Good bond to resin matrices
Carbon/Graphite Fibers:
- Highest strength and stiffness
- Limited esthetics (black appearance)
- Excellent fatigue resistance
- Superior mechanical properties
- Limited to non-esthetic applications
Clinical Applications
Direct Applications:
- Splinting of mobile teeth
- Periodontal splints
- Replacement of missing teeth
- Reinforcement of large restorations
- Post-orthodontic retention
Indirect Applications:
- Framework for bridges
- Reinforcement of provisional restorations
- Thin-walled crowns
- Maryland bridge frameworks
- Implant superstructures
Endodontic Applications:
- Prefabricated posts
- Custom fabricated posts
- Core reinforcement
- Post-endodontic restorations
- Alternative to metal posts
Technical Considerations
Fiber Architecture:
- Unidirectional fibers (highest strength in one direction)
- Bidirectional fibers (strength in two perpendicular directions)
- Woven fibers (balanced properties)
- Braided configurations (improved handling)
- Random orientation (isotropic properties)
Clinical Technique:
- Pre-impregnated vs. chairside impregnation
- Proper orientation for load-bearing
- Complete wetting with resin
- Adequate fiber quantity
- Protection from environmental exposure
CAD/CAM Composite Materials: Digital Workflow Integration
The digital revolution in dentistry has led to the development of specialized composite materials designed for milling and 3D printing.
Millable Composite Blocks
Material Characteristics:
- Industrial polymerization under controlled conditions
- Higher degree of conversion than direct materials
- Enhanced physical properties
- Homogeneous structure free of voids
- Optimized filler distribution
Advantages:
- Single-visit indirect restorations
- Reduced polymerization shrinkage issues
- Improved wear resistance
- Better marginal integrity
- More consistent results
Clinical Applications:
- Inlays and onlays
- Full crowns (especially posterior)
- Veneers
- Implant-supported crowns
- Long-term provisionals
Examples:
- VITA Enamic (VITA Zahnfabrik) - Polymer-infiltrated ceramic network
- Lava Ultimate (3M ESPE) - Resin nanoceramic
- Cerasmart (GC) - Force-absorbing hybrid ceramic
- Brilliant Crios (Coltene) - Reinforced composite block
3D-Printable Composites
Technology:
- Light-curable resin systems
- Layer-by-layer fabrication
- Digital design freedom
- Rapid manufacturing capability
- Continuously evolving formulations
Current Applications:
- Temporary crowns and bridges
- Surgical guides
- Occlusal splints
- Custom trays
- Emerging permanent restorations
Future Potential:
- Direct permanent restorations
- Custom shade-matched prosthetics
- Biomimetic tooth replacements
- Complex multi-material restorations
- On-demand manufacture of custom materials
Challenges:
- Material certification for permanent use
- Layer lines and surface finish
- Mechanical property limitations
- Biocompatibility concerns
- Post-processing requirements
Bioactive and Biomimetic Composites: The Biological Connection
Modern composite development increasingly focuses on materials that actively interact with biological tissues and mimic natural tooth structure.
Bioactive Glass-Containing Composites
Mechanism of Action:
- Release of calcium, phosphate, and fluoride ions
- Formation of hydroxyapatite layer
- Surface interaction with oral environment
- pH-buffering capabilities
- Potential integration with tooth structure
Clinical Benefits:
- Remineralization potential
- Reduced secondary caries risk
- Improved marginal integrity over time
- Self-repair capabilities at interfaces
- Enhanced biocompatibility
Examples:
- ACTIVA BioACTIVE (Pulpdent)
- Cention N (Ivoclar Vivadent)
- Beautifil II (Shofu Dental)
Biomimetic Approaches
Core Principles:
- Mimicking natural tooth structure
- Replicating dentin-enamel complex
- Gradient materials with varying properties
- Stress-dissipating interfaces
- Self-organizing structures
Current Developments:
- Interpenetrating phase composites
- Functionally graded materials
- Hierarchical structure replication
- Biomimetic adhesive interfaces
- Nature-inspired polymerization systems
Potential Benefits:
- More natural stress distribution
- Enhanced integration with tooth tissues
- Improved longevity through biomimetic principles
- Reduced interface failures
- Functional recovery of tooth properties
NEET Examination Tips for Advanced Composite Materials
For NEET MDS aspirants, advanced composite materials represent an evolving examination topic requiring current knowledge.
High-Yield Topics
- Bulk-fill composites: Technology, properties, and clinical applications
- Nanocomposite materials: Classifications and advantages
- Low-shrinkage technologies: Mechanisms and clinical significance
- Fiber-reinforced composites: Types and applications
- CAD/CAM composite materials: Properties and indications
Common NEET Questions
- Comparison between conventional and advanced composite systems
- Novel monomer systems and their advantages
- Classification of CAD/CAM composite materials
- Clinical applications of fiber-reinforced composites
- Technological principles behind reduced-shrinkage composites
Study Strategies
- Focus on understanding technological principles rather than brand names
- Create comparison charts of material properties
- Review the latest literature for clinical evidence
- Use flashcard technique for study of key innovations
- Review NEET previous year question papers for trend analysis
The Future of Dental Composites
Looking ahead, several promising trends are likely to shape the future development of dental composite materials:
Self-Adjusting Materials
Emerging Technologies:
- Composites with pressure-adaptive properties
- Materials that adjust hardness based on location
- Self-leveling systems
- Stimuli-responsive composites
- Environmental-adaptive materials
Potential Benefits:
- Simplified placement
- Reduced technique sensitivity
- Automatic adaptation to cavity irregularities
- Optimized properties for specific applications
- Reduced operator variability
Biomaterials Integration
Developing Approaches:
- Growth factor-releasing composites
- Cell-instructive materials
- Tissue engineering scaffolds
- Biodegradable components
- Stem cell interaction capabilities
Future Applications:
- Guided tissue regeneration
- Pulp-dentin complex regeneration
- Smart materials for vital pulp therapy
- Integration with regenerative endodontics
- Biomimetic tooth replacement
Interactive Diagnostic Capabilities
Innovative Features:
- Color-changing indicators for bacterial activity
- pH-responsive components for caries detection
- Stress-indicating properties
- Wear-monitoring capabilities
- Self-diagnostic features for replacement timing
Clinical Value:
- Early detection of restoration issues
- Patient motivation for oral hygiene
- Objective assessment of replacement need
- Preventive intervention opportunities
- Enhanced clinical decision-making
Conclusion
Advanced composite materials represent a rapidly evolving field that continues to transform restorative dentistry. From bulk-fill technologies that streamline placement to bioactive materials that interact with tooth tissues, these innovations are addressing traditional limitations while opening new clinical possibilities.
For dental professionals and NEET MDS aspirants, staying current with these developments is essential for both clinical excellence and examination success. As research continues, we can anticipate even more sophisticated materials that further enhance esthetics, function, and longevity while simplifying clinical procedures.
The future of dental composites lies in materials that not only restore teeth but actively contribute to oral health through bioactive properties, smart functionalities, and biomimetic designs. This exciting frontier promises to further transform the practice of restorative dentistry in the coming years.
This comprehensive overview serves as an essential revision tool for NEET candidates and a forward-looking reference for practitioners interested in emerging technologies in restorative dentistry.