Stress-Bearing Areas of Maxillary and Mandibular Arches
Medi Study Go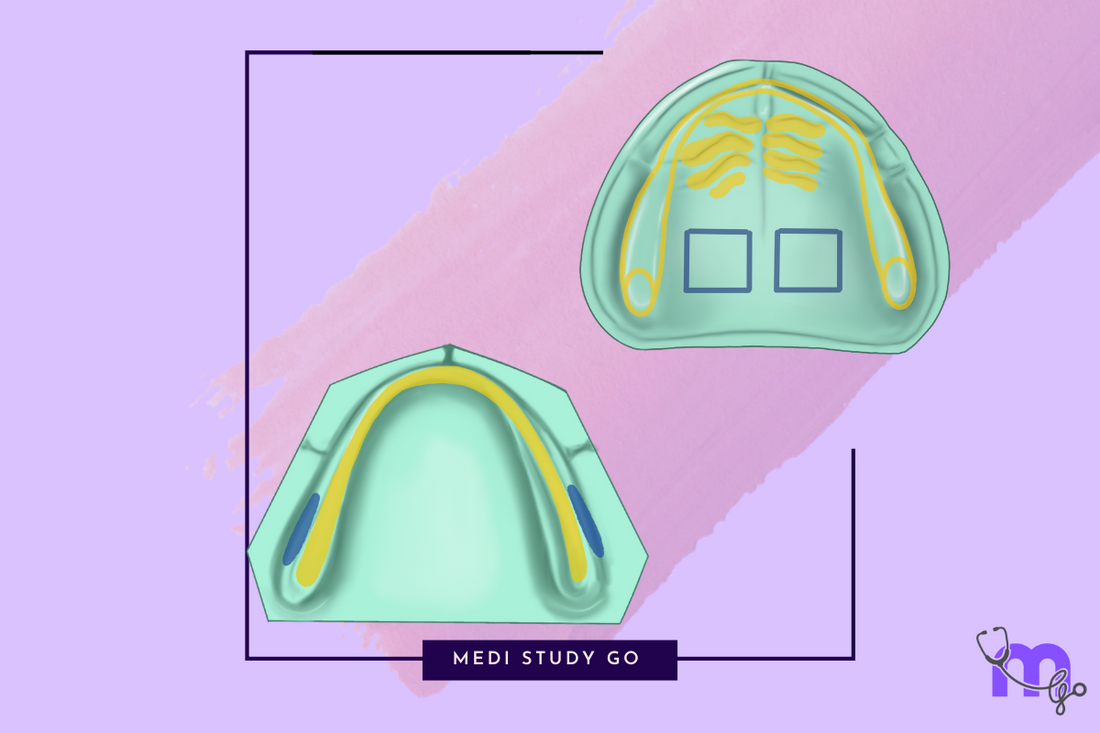
Related articles:
- Maxillary and Mandibular Landmarks: A Comprehensive Guide
- Maxillary Anatomical Landmarks: Detailed Examination
- Mandibular Anatomical Landmarks: Complete Guide
- Relief Areas in Maxillary and Mandibular Prosthetics
- Clinical Applications of Maxillary and Mandibular Landmarks
Basic Principles of Stress Distribution
Before diving into specific landmarks, let's establish some fundamental principles that guide stress distribution in denture design:
Tissue Resilience and Support Capacity
Not all oral tissues are created equal when it comes to bearing occlusal loads. Their capacity to support dentures depends on:
- Bone quality - Cortical bone provides better support than cancellous bone
- Mucosal thickness - Thin, firmly attached mucosa generally tolerates pressure better than thick, mobile tissue
- Underlying structures - Areas with neurovascular bundles or muscle attachments are poor stress-bearing regions
- Trabecular orientation - Bone trabeculae oriented perpendicular to pressure direction provide optimal support
Primary vs. Secondary Stress-Bearing Areas
We categorize stress-bearing areas into two groups:
Primary stress-bearing areas:
- Can tolerate significant occlusal forces
- Usually have cortical bone support
- Typically feature thin, firmly attached mucosa
- Should receive the majority of occlusal load
Secondary stress-bearing areas:
- Can tolerate moderate occlusal forces
- May have less optimal bone support
- Often feature thicker, more resilient mucosa
- Should receive less occlusal load than primary areas
Maxillary Stress-Bearing Areas

The maxilla offers multiple regions capable of supporting denture pressure, but their load-bearing capacity varies significantly.
Primary Stress-Bearing Areas in the Maxilla
Postero-lateral Slopes of Hard Palate
These slopes provide exceptional support due to:
- Considerable surface area for pressure distribution
- Bone trabecular pattern oriented perpendicular to the direction of force
- Capability to withstand tremendous occlusal pressure
In my experience, maximizing support from these slopes significantly enhances denture stability and patient comfort. I always demonstrate to students how these slopes form natural buttresses that resist both vertical and lateral displacement.
Maxillary Tuberosity
The maxillary tuberosity offers excellent support characteristics:
- Dense fibrous connective tissues with minimal compressibility
- Substantial bulk for pressure distribution
- Considerable support capacity for the posterior denture
However, its effectiveness depends on individual anatomy. Some patients present with flabby or hypermobile tuberosities that require modified impression techniques to ensure optimal support.
Crest of Residual Alveolar Ridge
While traditionally considered a primary stress-bearing area, the ridge's support capacity depends on:
- The degree of resorption
- The quality of remaining bone
- The thickness and resilience of covering tissues
The lateral walls of the ridges provide stability against lateral displacement and create a peripheral seal, enhancing denture retention.
A clinical pearl I share with students: As resorption progresses, the ridge becomes less reliable as a primary support area, necessitating greater reliance on the postero-lateral slopes of the hard palate.
Secondary Stress-Bearing Areas in the Maxilla
Rugae
The rugae provide secondary support with some limitations:
- They're covered thinly by soft tissues
- Their irregular folds of mucosa on the anterior palate are set at an angle to the residual ridge
- They resist forward movement of the denture
Interestingly, while rugae contribute to support, their primary function in denture stability is resistance to anteroposterior movement due to their orientation.
Mandibular Stress-Bearing Areas

The mandible presents greater challenges for stress distribution due to its smaller denture-bearing area and greater functional movement. Identifying and properly utilizing available support areas is critical for mandibular denture success.
Primary Stress-Bearing Area: Buccal Shelf
The buccal shelf represents the mandible's primary stress-bearing area due to several advantageous characteristics:
- Coverage by cortical bone
- Orientation at a right angle to the occlusal plane
- Excellent resistance to vertical occlusal forces
This structure has well-defined boundaries:
- Medially - Crest of residual ridge
- Anteriorly - Buccal frenum
- Laterally - External oblique ridge
- Distally - Retromolar pad
Utilizing the buccal shelf is often the key to resolving persistent instability in mandibular dentures. This area remains relatively stable even when the alveolar ridge undergoes significant resorption.
A technique to teach students: During impression-taking, apply selective pressure over the buccal shelf region to ensure optimal recording of this critical support area.
Secondary Stress-Bearing Area: Residual Alveolar Ridge
The residual alveolar ridge serves as a secondary support structure, with significant limitations:
- Edentulous mandibles are often extremely flat after resorption
- Ridge may be sharp, thin, or composed primarily of cancellous bone
- Ridge may contain large nutrient canals that are pressure-sensitive
These limitations result from the loss of the cortical layer of bone following tooth extraction. Nevertheless, the ridge contributes to overall denture support when utilized appropriately.
An important observation from my clinical experience:
As mandibular resorption progresses, the role of the residual ridge in denture support diminishes, while the importance of the buccal shelf increases proportionally. This understanding should guide impression techniques and pressure distribution strategies.
Clinical Assessment of Stress-Bearing Areas
Identifying stress-bearing areas requires systematic clinical assessment. Based on my experience, here are effective evaluation techniques:
Visual Examination
Start with thorough visual inspection, noting:
- Ridge height, width, and contour
- Mucosal color and texture (pale, firmly attached mucosa often indicates better support capacity)
- Presence of mobile tissue or inflamed areas
- Location of frena and muscle attachments
Palpation Techniques
Palpation provides critical information about tissue resilience and support capacity:
- Apply firm but gentle pressure to assess tissue compressibility
- Note areas of minimal displacement (good support) versus significant displacement (poor support)
- Identify bony prominences and undercuts
- Assess relative resilience between different regions
I teach students a systematic palpation approach, starting anteriorly and moving posteriorly while comparing left and right sides for asymmetry.
Functional Movement Assessment
Some support characteristics are only evident during function:
- Observe tissue movement during tongue function
- Note changes in vestibular depth during muscle contraction
- Assess soft palate movement to identify appropriate posterior extension
Diagnostic Imaging
While direct clinical examination is primary, radiographic assessment provides valuable supplementary information:
- Panoramic radiographs reveal overall ridge anatomy
- Cone beam CT scans show bone density and quality in stress-bearing regions
- Cephalometric analysis can indicate ridge resorption patterns
Impression Techniques for Optimal Stress Distribution
Different impression philosophies address stress distribution in various ways. Understanding these approaches helps clinicians select appropriate techniques for individual patients.
Selective Pressure Technique
This widely-used approach applies varying pressure to different oral regions:
- Maximum appropriate pressure on primary stress-bearing areas
- Moderate pressure on secondary stress-bearing areas
- Minimal pressure on relief areas
The goal is to distribute occlusal forces according to tissue support capacity.
Mucostatic Technique
This approach aims for minimal tissue displacement:
- Uses low-viscosity materials that record tissues in their resting state
- Minimizes pressure on all tissues
- May require occlusal adjustment to concentrate forces on stress-bearing areas
While theoretically sound, purely mucostatic techniques often result in inadequate border extension and compromised retention.
Functional Impression Technique
This philosophy records tissues under functional load:
- Uses border molding to capture tissues during movement
- May employ selective pressure principles during final impression
- Aims to distribute forces as they'll be experienced during function
I've found that combining elements of selective pressure and functional techniques yields the best results for most patients.
Common Clinical Challenges and Solutions
Even experienced clinicians encounter challenges related to stress distribution. Here are evidence-based approaches to common scenarios:
Flabby Ridge Tissue
When encountering mobile, displaceable tissue:
Impression approach:
- Use window technique to record flabby areas with minimal pressure
- Apply selective pressure to stable stress-bearing areas
- Consider two-material impression techniques
Prosthetic considerations:
- Design relieved areas beneath flabby tissue
- Concentrate occlusal forces on stable regions
- Consider soft liner in affected areas
Knife-Edge Ridges
Sharp, thin ridges present special challenges:
Management strategies:
- Distribute forces away from the crest to broader stress-bearing areas
- Consider surgical recontouring in severe cases
- Design dentures with broader bases to increase support area
- Employ tissue conditioning to improve denture-bearing surfaces
Severely Resorbed Mandible
When minimal ridge remains:
Approaches:
- Maximize extension to engage all available support areas
- Focus load distribution on the buccal shelf region
- Consider implant support when appropriate
- Employ neutral zone techniques to enhance stability
Importance for NEET MDS Examination
For students preparing for NEET MDS, stress-bearing areas represent high-yield examination topics. Based on NEET previous year question papers, focus on:
Commonly Tested Concepts
- Primary versus secondary stress-bearing areas - Their definitions, locations, and clinical significance
- Buccal shelf anatomy - Its boundaries and importance in mandibular denture support
- Postero-lateral slopes of the hard palate - Their anatomical characteristics and role in maxillary denture support
- Impression techniques - How different approaches address stress distribution
- Ridge resorption - How it affects stress distribution strategies
Application-Based Questions
NEET exams frequently include scenario-based questions such as:
- Identifying appropriate pressure application for specific oral regions
- Determining optimal impression techniques for challenging anatomies
- Selecting pressure-relief strategies for sensitive areas
Revision Strategies
Effective preparation includes:
- Creating comparison charts of primary and secondary stress-bearing areas
- Using flashcard techniques for study to reinforce key concepts
- Practicing with NEET mock tests that include clinical scenarios
- Reviewing NEET PYQs to understand common question formats
Advanced Concepts in Stress Distribution
For clinicians seeking deeper understanding, these advanced concepts provide additional insights:
Biomechanical Principles
The physics of stress distribution follows specific principles:
- Pressure = Force ÷ Area (increasing the supporting area decreases pressure)
- Compressive forces are better tolerated than shear forces
- Force direction should ideally be perpendicular to supporting tissues
- Broader distribution of forces generally results in better tissue tolerance
Understanding these principles helps clinicians make evidence-based decisions about denture design and occlusion.
Impact of Occlusal Schemes
Different occlusal philosophies affect stress distribution:
- Lingualized occlusion concentrates forces in primary stress-bearing areas
- Monoplane occlusion may reduce lateral forces but increases pressure per unit area
- Balanced occlusion distributes forces across multiple contact points
Selecting appropriate occlusal schemes based on individual anatomy can optimize stress distribution.
Dynamic versus Static Support
Support characteristics change during function:
- Tissues compress differently under dynamic versus static loads
- Functional movements can alter the effective supporting area
- Parafunctional habits may concentrate forces in unexpected regions
Considering both static and dynamic support factors leads to more successful prosthetic outcomes.
Clinical Implications for Denture Design
Understanding stress-bearing areas directly influences critical design decisions:
Base Thickness Variations
Denture base thickness should vary according to underlying support:
- Thinner over primary stress-bearing areas (to transmit forces)
- Thicker over relief areas (to distribute forces and prevent breakthrough)
- Reinforced in regions subjected to flexural stress
Strategic Use of Materials
Material selection can optimize stress distribution:
- Soft liners over sensitive or irregular areas
- Rigid bases over primary support regions
- Potentially employing mixed-material approaches for complex cases
Processing Considerations
Laboratory techniques influence final stress distribution:
- Compression molding may produce different pressure patterns than injection techniques
- Post-processing occlusal adjustment should respect underlying support capacity
- Selective grinding can redirect forces to appropriate support areas
Study Tips for Mastering Stress-Bearing Areas
For students preparing for examinations or clinicians refreshing their knowledge:
Effective Learning Approaches
- Create visual maps - Color-code different support areas on edentulous models
- Use the "teach-back" method - Explain concepts to peers to identify knowledge gaps
- Practice identification on casts - Marking stress-bearing areas on stone models reinforces understanding
- Correlate with clinical cases - Connect theoretical knowledge with real patient scenarios
- **Utilize NEET revision tools that emphasize support area identification
Recommended Resources
Beyond NEET preparation books, consider:
- Prosthodontic textbooks with clinical photos
- Journal articles discussing pressure distribution
- Clinical videos demonstrating impression techniques
- Last minute revision aids focusing on high-yield concepts
Conclusion
Mastering stress-bearing areas of maxillary and mandibular arches requires both theoretical knowledge and clinical judgment. Understanding which tissues can bear occlusal loads and which require relief is fundamental to successful prosthodontic treatment.
For students preparing for NEET MDS, these concepts represent core knowledge that appears frequently in examinations. Utilize NEET preparation books, flashcard applications for NEET, and regular practice with NEET mock tests to reinforce your learning.
For practicing clinicians, this knowledge guides critical decisions in impression-taking, denture design, and occlusal adjustment. Regular reassessment of these fundamental principles ensures continued clinical excellence.
Remember that each patient presents unique anatomical variations. The art of prosthodontics lies in applying these principles to individual cases, adapting techniques and designs to optimize comfort, function, and longevity.