Classification of Drugs Acting on ANS: A Complete Framework
Medi Study Go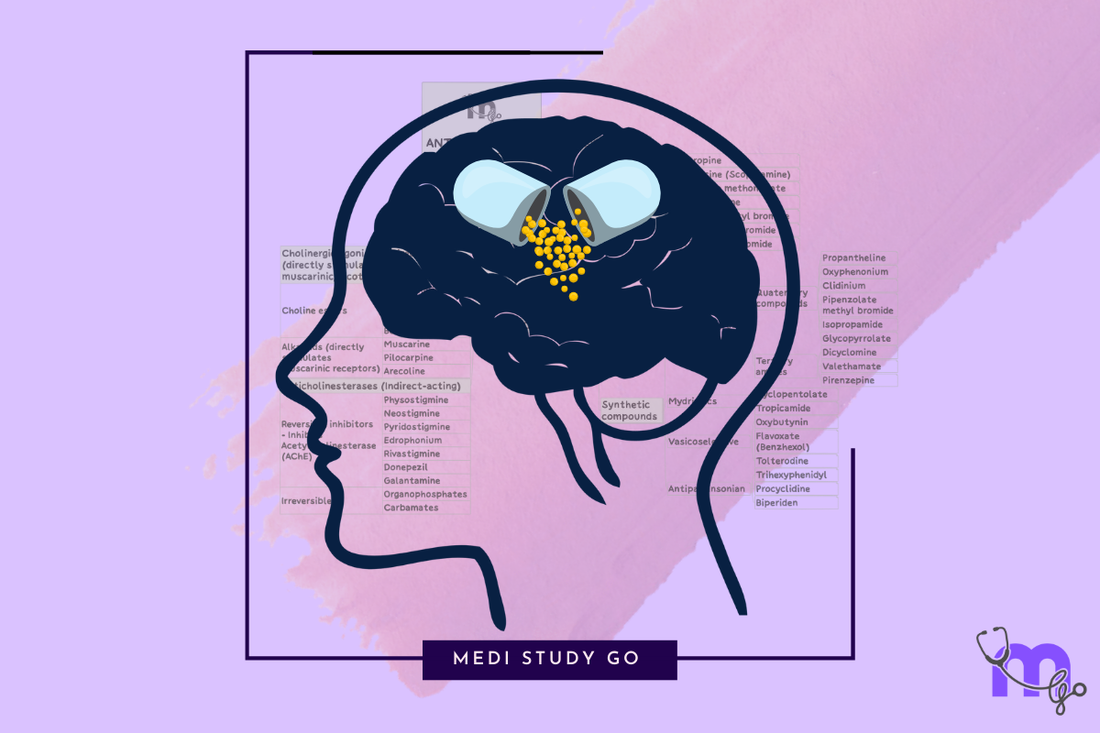
Understanding the classification of drugs that act on the autonomic nervous system (ANS) is essential for medical students, particularly those preparing for examinations like NEET. This organized framework helps in comprehending the complex interactions between drugs acting on ANS and their therapeutic applications.
Related resources in our ANS pharmacology series:
- Comprehensive Guide to Drugs Acting on the Autonomic Nervous System
- Understanding the Autonomic Nervous System: Foundation for Drug Action
- Cholinergic Drugs: Mechanisms and Clinical Applications
- Adrenergic Drugs: Mechanisms and Clinical Applications
- Screening Methods and Research Advances in ANS Pharmacology
Fundamentals of ANS Drug Classification
The classification of drugs acting on ANS is based on several key principles that reflect how these medications interact with the sympathetic and parasympathetic divisions. These organizing principles allow healthcare providers to predict drug effects, understand side effect profiles, and select appropriate therapies for various conditions.

Primary Classification Approaches
ANS drugs are classified using several complementary approaches:
1. Based on the Division of ANS Affected
Sympathetic (Adrenergic) System Drugs:
- Drugs that mimic or enhance sympathetic effects
- Drugs that block or inhibit sympathetic effects
Parasympathetic (Cholinergic) System Drugs:
- Drugs that mimic or enhance parasympathetic effects
- Drugs that block or inhibit parasympathetic effects
2. Based on the Type of Action
Mimetic Drugs (Agonists):
- Drugs that stimulate receptors and produce effects similar to natural neurotransmitters
Lytic Drugs (Antagonists):
- Drugs that block receptors and prevent the effects of natural neurotransmitters
3. Based on Receptor Specificity
Receptor-Selective Drugs:
- Target specific receptor subtypes (e.g., β₁-selective, M₃-selective)
Non-Selective Drugs:
- Act on multiple receptor subtypes simultaneously
4. Based on Site of Action
Presynaptic Drugs:
- Affect neurotransmitter synthesis, storage, release, or reuptake
Postsynaptic Drugs:
- Act directly on receptors on effector organs
Ganglionic Drugs:
- Act at the level of autonomic ganglia
![Classification Framework - Diagram showing major ANS drug classification categories]
Comprehensive Classification of ANS Drugs
A. Cholinergic (Parasympathetic) Drugs
1. Cholinergic Agonists (Parasympathomimetics)
a. Direct-Acting Cholinomimetics
-
Choline Esters:
- Acetylcholine (natural neurotransmitter, not used clinically due to rapid degradation)
- Methacholine (greater muscarinic selectivity)
- Carbachol (resistant to cholinesterase, mixed muscarinic/nicotinic action)
- Bethanechol (selective for muscarinic receptors, resistant to cholinesterase)
-
Alkaloids:
- Pilocarpine (selective muscarinic agonist, used for glaucoma)
- Muscarine (prototype muscarinic agonist, not used clinically)
- Nicotine (prototype nicotinic agonist, not used therapeutically)
b. Indirect-Acting Cholinomimetics (Anticholinesterases)
-
Reversible Inhibitors:
- Physostigmine (tertiary amine, crosses blood-brain barrier)
- Neostigmine (quaternary amine, limited CNS penetration)
- Pyridostigmine (longer duration than neostigmine)
- Edrophonium (ultra-short acting, used diagnostically)
- Rivastigmine, Donepezil, Galantamine (used for Alzheimer's disease)
-
Irreversible Inhibitors:
- Organophosphates (echothiophate, insecticides, nerve agents)
- Carbamates (certain insecticides)
2. Cholinergic Antagonists (Parasympatholytics)
a. Muscarinic Receptor Antagonists
-
Non-selective:
- Atropine (prototype, naturally occurring belladonna alkaloid)
- Scopolamine (greater central effects than atropine)
- Ipratropium (quaternary derivative, limited systemic absorption)
- Glycopyrrolate (quaternary compound with limited CNS effects)
-
M₁-selective:
- Pirenzepine (used for peptic ulcer)
- Telenzepine (investigational)
-
M₃-selective:
- Darifenacin (bladder selectivity)
- Solifenacin (used for overactive bladder)
b. Nicotinic Receptor Antagonists
-
Ganglionic Blockers:
- Hexamethonium (historical compound, not used clinically)
- Mecamylamine (can cross blood-brain barrier)
- Trimethaphan (ultra-short acting, used in controlled hypotension)
-
Neuromuscular Blockers:
- Tubocurarine (non-depolarizing)
- Pancuronium, Vecuronium, Rocuronium (synthetic non-depolarizing agents)
- Succinylcholine (depolarizing blocker)
B. Adrenergic (Sympathetic) Drugs
1. Adrenergic Agonists (Sympathomimetics)
a. Direct-Acting Sympathomimetics
-
Catecholamines:
- Epinephrine (non-selective α and β agonist)
- Norepinephrine (strong α, moderate β₁, minimal β₂ activity)
- Dopamine (dose-dependent receptor activation)
- Isoproterenol (non-selective β agonist, minimal α activity)
-
Non-catecholamines:
- Phenylephrine (selective α₁ agonist)
- Clonidine, Methyldopa (α₂ agonists)
- Albuterol, Terbutaline (selective β₂ agonists)
- Dobutamine (predominantly β₁ agonist)
- Ritodrine (β₂ agonist used for tocolysis)
- Mirabegron (β₃ agonist for overactive bladder)
b. Indirect-Acting Sympathomimetics
- Amphetamine (release of NE, some dopamine effects)
- Tyramine (releases stored NE)
- Cocaine (inhibits NE reuptake)
- Various tricyclic antidepressants (inhibit NE reuptake)
c. Mixed-Action Sympathomimetics
- Ephedrine (direct + indirect effects)
- Pseudoephedrine (less CNS effect than ephedrine)
- Metaraminol (predominantly indirect with some direct action)
2. Adrenergic Antagonists (Sympatholytics)
a. α-Adrenergic Blockers
-
Non-selective α-blockers:
- Phenoxybenzamine (irreversible)
- Phentolamine (reversible)
-
Selective α₁-blockers:
- Prazosin (prototype)
- Terazosin, Doxazosin (longer-acting)
- Tamsulosin, Silodosin (uroselectivity for BPH)
-
Selective α₂-blockers:
- Yohimbine
- Mirtazapine (also has other actions)
b. β-Adrenergic Blockers
-
Non-selective β-blockers:
- Propranolol (prototype)
- Nadolol (longer-acting)
- Timolol (used topically for glaucoma)
- Pindolol, Penbutolol (partial agonist activity)
-
Selective β₁-blockers (Cardioselective):
- Metoprolol
- Atenolol
- Bisoprolol
- Nebivolol (also has nitric oxide-mediated vasodilation)
c. Mixed α/β-Blockers:
- Labetalol (α₁ and non-selective β antagonist)
- Carvedilol (α₁, β₁, and β₂ antagonist)
C. Drugs Affecting Neurotransmitter Disposition
1. Synthesis Inhibitors
- Metyrosine (inhibits tyrosine hydroxylase, reducing catecholamine synthesis)
2. Storage Inhibitors
- Reserpine (depletes catecholamine storage vesicles)
- Tetrabenazine (similar to reserpine but shorter acting)
3. Release Inhibitors
- Guanethidine (blocks NE release, now rarely used)
- Bretylium (blocks NE release, historical antiarrhythmic)
4. Reuptake Inhibitors
- Cocaine (increases sympathetic activity by blocking NE reuptake)
- Atomoxetine (selective norepinephrine reuptake inhibitor)
5. Metabolism Inhibitors
- MAO inhibitors (increase NE availability by inhibiting breakdown)
- COMT inhibitors (entacapone, tolcapone - primarily used for dopamine metabolism in Parkinson's)
Clinical Applications Based on Classification
Understanding the classification of ANS drugs directly translates to their therapeutic applications:
Cholinergic Agonist Applications
- Direct-acting: Urinary retention, glaucoma, GI/bladder atony
- Anticholinesterases: Myasthenia gravis, glaucoma, Alzheimer's disease, reversal of neuromuscular blockade
Anticholinergic Applications
- Preoperative medication (reduce secretions)
- Motion sickness
- Parkinson's disease (reduce tremor)
- Overactive bladder
- Bronchodilation in COPD/asthma
- Mydriasis and cycloplegia for eye examinations
Sympathomimetic Applications
- Anaphylaxis (epinephrine)
- Hypotension/shock (various vasopressors)
- Cardiac arrest (epinephrine)
- Bronchospasm (β₂ agonists)
- Nasal congestion (α agonists)
- ADHD (indirect sympathomimetics)
- Glaucoma (α₂ agonists reduce aqueous humor production)
Sympatholytic Applications
- α-blockers: Hypertension, BPH, pheochromocytoma
- β-blockers: Hypertension, angina, arrhythmias, heart failure, glaucoma, migraine prophylaxis
- Combined α/β-blockers: Hypertension, pheochromocytoma
Special Considerations for Drug Selection
The classification framework helps guide drug selection based on several important factors:
Receptor Selectivity Considerations
-
Selective agents may reduce certain adverse effects
- Example: Cardioselective β-blockers (β₁) have less effect on bronchial smooth muscle (β₂)
- Example: Uroselectivity of tamsulosin reduces cardiovascular side effects
Route of Administration
- Some agents have limited oral bioavailability
- Quaternary ammonium compounds generally don't cross blood-brain barrier
- Topical administration (eye drops, inhalers) may limit systemic effects
Duration of Action
- Clinical situation may require short-acting or long-acting agents
- Emergency situations (anaphylaxis) vs. chronic management (hypertension)
Partial Agonist Properties
- Some antagonists have intrinsic sympathomimetic activity (ISA)
- May be beneficial in patients where complete blockade is undesirable
Clinical Relevance of ANS Drug Classification for NEET Exam
Understanding the classification of drugs acting on ANS is particularly important for NEET examinations:
High-Yield Classification Topics
- Receptor subtype selectivity of major drugs
- Mechanism-based classification systems
- Prototype drugs for each category
- Clinical applications based on classification
- Adverse effects predicted by receptor activity profile
Practice Applications
- Predicting which drug might be preferred in specific clinical scenarios
- Understanding why certain drug combinations are synergistic or antagonistic
- Recognizing adverse effects based on receptor profile
- Explaining contraindications based on receptor activity
Recent Advances in ANS Drug Classification
The traditional classification framework continues to evolve with new insights:
Newer Receptor Subtypes
- Additional adrenergic and cholinergic receptor subtypes identified
- Greater understanding of receptor signaling pathways
Novel Therapeutic Targets
- Allosteric modulators of ANS receptors
- Biased agonists that activate specific signaling pathways
- Combination therapies targeting complementary mechanisms
Personalized Medicine Approaches
- Pharmacogenetic variations affecting drug response
- Receptor polymorphisms influencing efficacy and side effects
Conclusion
The classification of drugs acting on ANS provides a comprehensive framework for understanding how these medications work, predicting their effects, and making informed therapeutic decisions. For students preparing for NEET and other medical examinations, mastering this classification system is essential for success in pharmacology and future clinical practice.
This classification system doesn't exist in isolation but is intimately connected to the physiology of the autonomic nervous system and the detailed mechanisms of drug action. By understanding how drugs are classified, students and healthcare professionals can better navigate the complex world of autonomic nervous system drugs and their applications in patient care.