Oral Manifestations of Diabetes Mellitus
Medi Study Go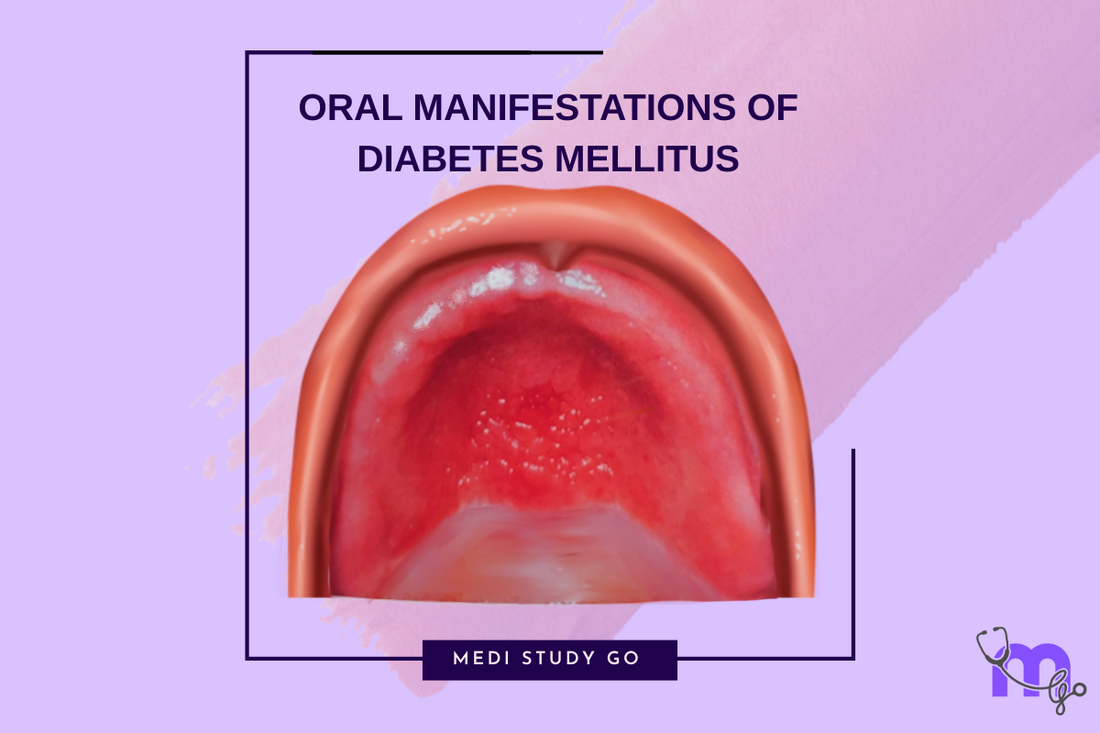
Related Resources:
- Dental Management of Diabetes Mellitus: Comprehensive Guide
- Diabetes Mellitus Treatment Considerations for Dental Professionals
- Managing Diabetic Emergencies in the Dental Office
- Periodontal Disease and Diabetes: A Bidirectional Relationship
- Comprehensive Care Approach for Diabetic Dental Patients
This comprehensive review of diabetes-related oral manifestations is essential for NEET MDS preparation. Many concepts covered here frequently appear in NEET previous year question papers. Use this guide alongside your NEET preparation books for thorough exam readiness.
Introduction

The oral cavity often reveals significant signs of systemic conditions, making it a valuable diagnostic window for healthcare providers. In patients with diabetes mellitus, characteristic oral manifestations frequently develop, especially in cases of poor glycemic control. Understanding these manifestations is crucial for dental professionals to provide appropriate care and potentially contribute to early diagnosis of undiagnosed diabetes.
This guide provides a comprehensive overview of the diverse oral manifestations associated with diabetes mellitus, their clinical presentation, pathophysiological basis, and implications for dental management.
Pathophysiological Basis of Oral Manifestations
The pathophysiology of diabetes mellitus creates conditions that significantly impact oral health through several mechanisms:
- Microangiopathy affecting small blood vessels in oral tissues
- Impaired wound healing due to altered collagen metabolism
- Decreased salivary flow resulting from polyuria and dehydration
- Compromised immune response leading to increased infection susceptibility
- Formation of advanced glycation end products (AGEs) affecting tissue integrity
- Altered oral microbiome composition and balance
Common Oral Manifestations of Diabetes Mellitus
Periodontal Disease
Periodontal disease is widely recognized as the "sixth complication" of diabetes mellitus. Diabetic patients show:
- Earlier onset and increased severity of gingivitis
- More rapid progression to periodontitis
- Greater attachment loss and alveolar bone destruction
- Higher prevalence of deep periodontal pockets
- Increased tooth mobility and subsequent tooth loss
In uncontrolled diabetes, periodontal destruction accelerates due to exaggerated inflammatory responses, reduced neutrophil function, and impaired tissue repair mechanisms. Notably, successful management of periodontal disease can positively impact glycemic control, highlighting the bidirectional relationship between these conditions.
Xerostomia (Dry Mouth)
Dry mouth affects approximately 40-80% of diabetic patients and results from:
- Polyuria causing systemic dehydration
- Autonomic neuropathy affecting salivary gland innervation
- Microvascular changes within salivary glands
- Side effects of medications used to treat diabetes or its complications
Clinical symptoms include oral burning sensation, difficulty swallowing, altered taste perception, and increased caries risk. Reduced salivary flow also compromises the mouth's natural antimicrobial properties, further elevating infection risk.
Oral Candidiasis
Diabetes predisposes individuals to fungal infections, particularly oral candidiasis, through multiple mechanisms:
- Increased salivary glucose levels creating favorable growth conditions
- Impaired neutrophil function
- Reduced salivary flow
- Altered local immunity
Common presentations include:
- Pseudomembranous candidiasis: White plaques that can be wiped off
- Erythematous candidiasis: Red patches typically on the palate or tongue
- Angular cheilitis: Painful cracks at the corners of the mouth
- Median rhomboid glossitis: Characteristic diamond-shaped lesion on the dorsum of tongue
Burning Mouth Syndrome
Many diabetic patients report unexplained burning sensations, particularly on the tongue. This manifestation may arise from:
- Peripheral neuropathy affecting oral sensory nerves
- Xerostomia
- Undiagnosed candidiasis
- Medication side effects
The burning sensation typically affects the anterior two-thirds of the tongue, palate, and lips, often intensifying throughout the day.
Taste Disturbances
Approximately 33% of poorly controlled diabetic patients experience taste alterations, including:
- Diminished taste perception (hypogeusia)
- Distorted taste (dysgeusia)
- Persistent metallic taste
- Sweet taste disorder
These disturbances result from peripheral neuropathy affecting taste receptors, salivary dysfunction, and altered oral microbiome.
Delayed Wound Healing
Impaired wound healing in the oral cavity of diabetic patients manifests as:
- Prolonged post-extraction healing time
- Increased incidence of dry socket following extractions
- Delayed mucosal healing after periodontal surgery
- Higher risk of post-surgical infections
This delayed healing stems from microangiopathy, impaired collagen synthesis, reduced growth factor production, and compromised immune response.
Other Significant Oral Manifestations
Lichen Planus and Lichenoid Reactions
Diabetic patients show higher prevalence of oral lichen planus and lichenoid reactions, characterized by:
- White reticular patterns on the buccal mucosa
- Erosive or ulcerative lesions
- Gingival desquamation
Oral Hypoglycemic Medication Effects
Some oral hypoglycemic agents can cause:
- Lichenoid drug reactions
- Erythema multiforme
- Taste alterations
- Gingival enlargement (particularly with calcium channel blockers often prescribed for diabetic patients with hypertension)
Increased Dental Caries Risk
Factors contributing to elevated caries risk include:
- Salivary dysfunction
- Higher glucose levels in gingival crevicular fluid
- Poor glycemic control affecting immune function
- Altered dietary habits
Clinical Implications and Diagnostic Value
Recognizing these oral manifestations serves several important purposes:
- Early detection of undiagnosed diabetes: Dental professionals may be the first to identify signs suggesting undiagnosed diabetes, prompting appropriate medical referral
- Assessment of glycemic control: Certain oral manifestations, particularly recurrent or persistent candidiasis and rapidly progressing periodontal disease, may indicate poor glycemic control
- Treatment planning modifications: Awareness of these manifestations guides appropriate treatment planning, including prophylactic measures and surgical approach modifications
- Interdisciplinary collaboration: Identification of significant oral manifestations facilitates communication with medical providers regarding a patient's overall diabetes management
Diagnostic Approach
When encountering suspicious oral manifestations, dental professionals should:
- Conduct thorough medical history review, including:
- Family history of diabetes
- Classic symptoms (polydipsia, polyuria, polyphagia)
- Recent weight changes
- Current medications
- Perform comprehensive oral examination focusing on:
- Periodontal status assessment
- Salivary flow evaluation
- Mucosal integrity examination
- Candidal infection screening
- Consider appropriate laboratory testing:
- In-office blood glucose screening
- HbA1c testing when available
- Medical referral for definitive diagnosis
Conclusion
The diverse oral manifestations of diabetes mellitus represent important clinical signs that dental professionals should recognize and address. Beyond their local significance, these manifestations often reflect the patient's systemic health status and glycemic control.
Dental practitioners play a crucial role in early detection of undiagnosed cases and monitoring of disease progression. By understanding the pathophysiological basis and clinical presentation of these oral manifestations, dental professionals can contribute significantly to comprehensive diabetes care through appropriate dental management and timely medical referrals.
For students preparing for NEET MDS examinations, thorough knowledge of these manifestations and their underlying mechanisms represents essential content frequently tested in NEET previous year question papers.