Metal-Ceramic Systems and Ceramic Failures
Medi Study Go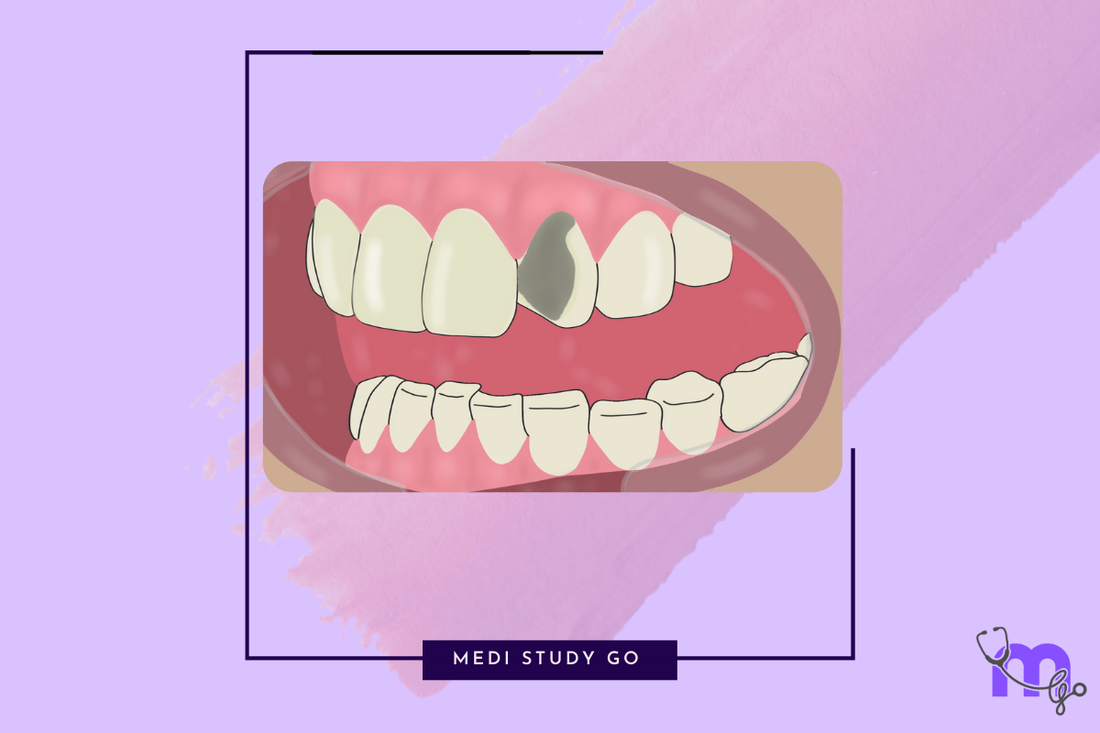
Related Resources:
- Dental Ceramics: A Comprehensive Guide
- Types and Classification of Dental Ceramics
- Fabrication Techniques for Dental Ceramics
- Properties and Strengthening Methods of Dental Ceramics
- Clinical Applications of Dental Ceramics
Introduction to Metal-Ceramic Restorations
Metal-ceramic restorations (also known as porcelain-fused-to-metal or PFM) remain a cornerstone of restorative dentistry despite the growing popularity of all-ceramic systems. For NEET MDS aspirants, understanding these traditional yet enduring restorations is essential, as they frequently appear in NEET previous year question papers and clinical scenarios.
This comprehensive guide explores metal-ceramic systems, including their composition, bonding mechanisms, clinical applications, and common failure modes. We'll also examine ceramic restoration failures broadly to support thorough NEET preparation and clinical problem-solving abilities.
Metal-Ceramic Bonding Mechanisms
The success of metal-ceramic restorations depends on the durable bond between the metal substructure and overlying ceramic. This bonding occurs through multiple mechanisms that are frequently tested in NEET exam questions.
Mechanical Bonding
-
Micro-Mechanical Retention
- Surface roughness created through:
- Grinding with rotary instruments
- Airborne-particle abrasion (50-100 μm Al₂O₃)
- Chemical etching
- Provides mechanical interlocking between metal and ceramic
- Surface roughness created through:
-
Macro-Mechanical Design Features
- Retention beads, loops, or mesh
- Retentive grooves or undercuts
- Less common in modern systems
-
Compressive Forces
- Created by differential thermal contraction
- Metal's higher coefficient of thermal expansion creates compression on ceramic during cooling
- Enhances mechanical retention
Chemical Bonding
-
Oxide Layer Formation
- Metal oxidation during degassing or initial firing
- Controlled oxide layer thickness critical:
- Too thin: insufficient bond
- Too thick: weakened bond
- Oxides bond with silicon dioxide in ceramic
-
Van der Waals Forces
- Secondary forces between metal and ceramic molecules
- Contribute to overall bond strength
- Enhanced by wetting of metal by ceramic
-
Ionic and Covalent Bonds
- Primary chemical bonds
- Form between metal oxides and ceramic components
- Essential for long-term bond durability
Factors Affecting Bond Strength
-
Metal Surface Treatment
- Sandblasting: Creates micromechanical retention
- Degassing: Controls oxide layer formation
- Contamination: Must be avoided (oils, debris)
-
Ceramic Application Technique
- Proper condensation reduces firing shrinkage
- Adequate wetting of metal surface
- Application of opaque layer
-
Thermal Compatibility
- Coefficient of thermal expansion (CTE) matching
- Typically metal CTE slightly higher than ceramic
- Mismatch leads to stresses and failure
Metal Substructure Materials
High Noble Alloys (Gold-Based)
-
Composition
- Gold (Au): 75-90%
- Platinum (Pt): 0-10%
- Palladium (Pd): 0-10%
- Silver (Ag): 0-10%
- Trace elements: Cu, Zn, In, Sn
-
Properties
- Excellent biocompatibility
- Good bond strength with ceramic
- High corrosion resistance
- Controlled oxide formation
- CTE: 14-15 × 10⁻⁶/°C
-
Advantages and Limitations
- Advantages: Proven track record, excellent fit, biocompatibility
- Limitations: High cost, yellow color may show through thin ceramic
Noble Alloys (Palladium-Based)
-
Composition
- Palladium (Pd): 50-60%
- Silver (Ag): 30-35% (in Pd-Ag alloys)
- Gold (Au): 5-15%
- Trace elements: In, Sn, Ga
-
Properties
- Good biocompatibility
- Adequate bond strength
- Moderate corrosion resistance
- CTE: 14-15 × 10⁻⁶/°C
-
Advantages and Limitations
- Advantages: Lower cost than high noble, good physical properties
- Limitations: Silver can cause ceramic discoloration (greening)
Base Metal Alloys
-
Nickel-Chromium Alloys
- Composition:
- Nickel (Ni): 60-80%
- Chromium (Cr): 10-27%
- Molybdenum (Mo): 4-10%
- Other: Be, Al, Si
- Properties:
- High strength and hardness
- Good bond strength with proper oxidation
- CTE: 13.5-14.5 × 10⁻⁶/°C
- Concerns: Nickel allergies, beryllium toxicity
- Composition:
-
Cobalt-Chromium Alloys
- Composition:
- Cobalt (Co): 55-65%
- Chromium (Cr): 25-35%
- Molybdenum (Mo): 4-5%
- Other: W, Si, Mn
- Properties:
- Highest modulus of elasticity
- Excellent corrosion resistance
- CTE: 14-15 × 10⁻⁶/°C
- Advantages: No nickel, higher biocompatibility than Ni-Cr
- Composition:
Key Requirements for Metal Substructures
-
Technical Requirements
- Adequate strength to support ceramic
- Proper oxide formation for bonding
- Compatible CTE (slightly higher than ceramic)
- Sufficient rigidity (minimum 0.3-0.5mm thickness)
-
Design Considerations
- Uniform support for ceramic
- No sharp angles or transitions
- Thicker metal in stress-bearing areas
- Collar/metal margin in non-esthetic areas
Porcelain Used in Metal-Ceramics
Types of Porcelain for Metal-Ceramics
-
Feldspathic Porcelain
- Most common type
- Composition:
- Feldspar (potassium aluminosilicate)
- Quartz (silica)
- Kaolin (hydrated aluminum silicate)
- Properties:
- CTE: 12-14 × 10⁻⁶/°C
- Firing temperature: 850-1000°C
- Excellent esthetics
-
Leucite-Reinforced Porcelain
- Contains leucite (KAlSi₂O₆) crystals
- Higher strength than conventional feldspathic
- Controlled leucite content adjusts CTE
Layering Ceramics for Metal-Ceramic Restorations
-
Opaque Layer
- Purpose: Masks metal color, initiates bonding
- Composition: High content of opacifying oxides (titanium, tin, zirconium)
- Application: Thin layers (0.2-0.3mm total)
-
Dentin (Body) Layer
- Purpose: Provides basic tooth color and form
- Composition: Moderate translucency feldspathic porcelain
- Properties: Balances translucency and opacity
-
Enamel Layer
- Purpose: Creates translucent outer layer
- Composition: Higher glass content, lower opacity
- Properties: Higher translucency, mimics natural enamel
-
Effect Materials
- Purpose: Creates characterization
- Types: Stains, opalescent porcelains, fluorescent modifiers
Glass Modifiers in Metal-Ceramic Porcelains
-
Flux Components
- Potassium oxide (K₂O)
- Sodium oxide (Na₂O)
- Lower fusion temperature
-
Opacity Modifiers
- Titanium oxide (TiO₂)
- Zirconium oxide (ZrO₂)
- Tin oxide (SnO₂)
-
Color Modifiers
- Iron oxide: brown/yellow
- Copper oxide: green
- Manganese oxide: lavender
- Cobalt oxide: blue
Tooth Preparation Requirements for Metal-Ceramics

Understanding preparation guidelines is essential for NEET mock tests and clinical competence with metal-ceramic restorations.
Facial/Buccal Surface
- Reduction amount: 1.2-1.5mm
- Margin design: Shoulder or chamfer
- Purpose: Provides space for opaque and esthetic ceramic layering
Lingual/Palatal Surface
- Reduction amount: 0.5-1.0mm
- Margin design: Chamfer
- Purpose: Provides metal support and strength
Occlusal/Incisal Surface
- Reduction amount: 1.5-2.0mm
- Margin design: Beveled or rounded
- Purpose: Ensures adequate clearance for strength
Proximal Surface
- Reduction amount: 1.0-1.5mm
- Margin design: Shoulder or chamfer
- Purpose: Ensures proper contour and esthetics
Margin Placement
- Location: Supragingival/subgingival
- Design: Shoulder in esthetic areas
- Purpose: Maintains periodontal health and esthetics
Advantages and Limitations of Metal-Ceramic Restorations
Advantages
-
High strength and fracture resistance
- Metal substructure provides excellent support
- Lower failure rates in high-stress areas
- Suitable for long-span bridges
-
Good esthetics with proper ceramic layering
- Capable of excellent esthetics with skilled technicians
- Various opacity and translucency options
- Can mimic natural tooth appearance
-
Biocompatibility and longevity
- Excellent track record (over 50 years)
- Predictable clinical performance
- Well-documented clinical research
Limitations
-
Requires significant tooth reduction
- More invasive than some all-ceramic options
- Necessary to accommodate both metal and ceramic
-
Esthetic limitations compared to all-ceramic
- Metal may show through thin ceramic
- Potential for gingival discoloration
- Limited translucency at margin areas
-
Risk of ceramic chipping
- Veneer fracture common complication
- Requires adequate thickness and support
- Repair often challenging
Failure Modes and Prevention in Metal-Ceramic Restorations

Understanding failure mechanisms is crucial for both NEET MDS examinations and clinical practice.
Common Failures
-
Ceramic Fracture
- Most common failure mode
- Types:
- Cohesive fracture within ceramic
- Adhesive fracture at metal-ceramic interface
- Contributing factors:
- Inadequate support
- Excessive occlusal forces
- Improper design or thickness
-
Debonding from Metal
- Separation of ceramic from metal substructure
- Causes:
- Improper surface treatment
- Contamination
- CTE mismatch
- Excessive oxide layer
-
Marginal Discrepancies
- Gap formation between restoration and tooth
- Leads to microleakage, secondary caries
- Causes:
- Improper fit
- Multiple firing cycles
- Improper cementation
Prevention Strategies
-
Proper Metal Design
- Adequate thickness (0.3-0.5mm)
- No sharp angles
- Uniform support for ceramic
- Framework verification before ceramic application
-
Controlled Firing Cycles
- Follow manufacturer recommendations
- Proper temperature and hold times
- Avoid excessive firings that may weaken bond
-
Avoid Sharp Angles in Preparation
- Reduces stress concentration
- Improves load distribution
- Prevents ceramic fracture
-
Occlusal Adjustment and Protection
- Proper occlusal scheme
- Avoid heavy contacts on ceramic
- Night guards for parafunctional patients
General Ceramic Restoration Failures
Beyond metal-ceramics, understanding broader ceramic failure patterns is important for comprehensive NEET preparation.
Failure Patterns in All-Ceramic Systems
-
Catastrophic Fracture
- Complete restoration failure
- More common in:
- Feldspathic crowns
- Inadequate thickness
- High-stress locations
- Prevention:
- Appropriate material selection
- Adequate thickness
- Proper support
-
Chip Fractures
- Partial loss of ceramic material
- Common in:
- Layered zirconia restorations
- Areas of occlusal contact
- Prevention:
- Monolithic designs in high-stress areas
- Proper cooling protocols
- Anatomic framework support
-
Marginal Failures
- Chipping or fracture at margins
- Common in thin areas
- Prevention:
- Proper margin design
- Adequate thickness at margins
- Proper handling during try-in
Material-Specific Failure Patterns
-
Feldspathic and Leucite-Reinforced Ceramics
- Primarily bulk fractures
- Often related to inadequate thickness
- Higher failure rates in posterior regions
-
Lithium Disilicate
- Chip fractures more common than catastrophic failures
- Connector fractures in bridges
- Generally good clinical performance
-
Zirconia-Based Restorations
- Monolithic: Rare fractures, occasional chip-offs
- Layered: Veneer chipping most common failure
- Framework fractures rare with proper design
-
CAD/CAM Ceramics
- Milling defects can initiate cracks
- Material- and system-specific failures
- Processing flaws more significant than with conventional techniques
Contributing Factors to Ceramic Failures
-
Biological Factors
- Poor oral hygiene
- Periodontal disease
- Secondary caries
- Pulpal complications
-
Mechanical Factors
- Parafunctional habits
- Improper occlusal schemes
- Inadequate design
- Material selection errors
-
Technical Factors
- Processing errors
- Firing irregularities
- Contamination
- Improper handling
-
Clinical Factors
- Improper preparation
- Inadequate isolation during cementation
- Cement selection errors
- Improper try-in or adjustment
Clinical Management of Ceramic Failures
Understanding failure management is important for comprehensive NEET preparation and clinical competence.
Evaluation of Failed Restorations
-
Failure Analysis
- Identify failure mode and location
- Determine contributing factors
- Assess restorability
-
Documentation
- Clinical photographs
- Radiographic examination
- Patient symptoms and history
Repair Options
-
Intraoral Repair
- Indications:
- Minor chipping
- Areas accessible for proper conditioning
- Patient factors prohibiting replacement
- Procedure:
- Surface roughening
- Silane application (for glass ceramics)
- Adhesive application
- Composite addition
- Indications:
-
Laboratory Repair
- Indications:
- Moderate damage
- Retrievable restoration
- Procedures:
- Addition of new ceramic material
- Not always predictable
- May require rebonding
- Indications:
-
Replacement
- Indications:
- Major fractures
- Multiple or recurrent failures
- Esthetic concerns
- Considerations:
- Re-evaluation of material choice
- Reassessment of occlusion
- Possible design modifications
- Indications:
Prevention of Future Failures
-
Material Selection Considerations
- Higher strength materials for high-stress areas
- Monolithic designs for bruxers
- Layered ceramics only in low-stress areas
-
Design Modifications
- Increased thickness
- Modified occlusal scheme
- Protective splints for parafunctional habits
-
Processing Improvements
- Controlled cooling protocols
- Proper laboratory communication
- Quality control measures
NEET MDS Exam Focus Points
For effective last minute revision and success in NEET mock tests, focus on these high-yield points:
-
Metal-Ceramic Bonding Mechanisms
- Mechanical vs. chemical bonding
- Oxide layer formation and significance
- Factors affecting bond strength
-
Metal Alloy Composition and Properties
- High noble vs. noble vs. base metal
- Advantages and limitations of each
- Indications for specific alloys
-
Preparation Requirements
- Reduction amounts for different surfaces
- Margin designs and purposes
- Common preparation errors
-
Failure Modes and Causes
- Types of ceramic fractures
- Contributing factors to failures
- Prevention strategies
-
Comparative Aspects
- Metal-ceramic vs. all-ceramic advantages/limitations
- Cost-benefit considerations
- Longevity and survival rates
-
Clinical Decision-Making
- Case selection criteria
- Material selection principles
- Management of complications
Conclusion
Metal-ceramic restorations remain clinically relevant despite advances in all-ceramic systems. Their combination of strength, durability, and acceptable esthetics ensures their continued use in many clinical situations. For NEET MDS aspirants, understanding both traditional metal-ceramic systems and modern all-ceramic alternatives, along with their respective failure patterns, is essential for examination success and future clinical practice.
By mastering the bonding mechanisms, material properties, preparation requirements, and failure modes discussed in this guide, you'll be well-equipped to approach related questions in the NEET exam. Combine this knowledge with information from our related guides on ceramic types, properties, fabrication techniques, and clinical applications for comprehensive understanding of dental ceramics.
Regular practice with NEET previous year question papers and targeted NEET preparation using flashcard techniques for study will help reinforce these concepts and identify areas requiring further review.