Common Infectious Diseases: Pathophysiology and Clinical Presentations
Medi Study Go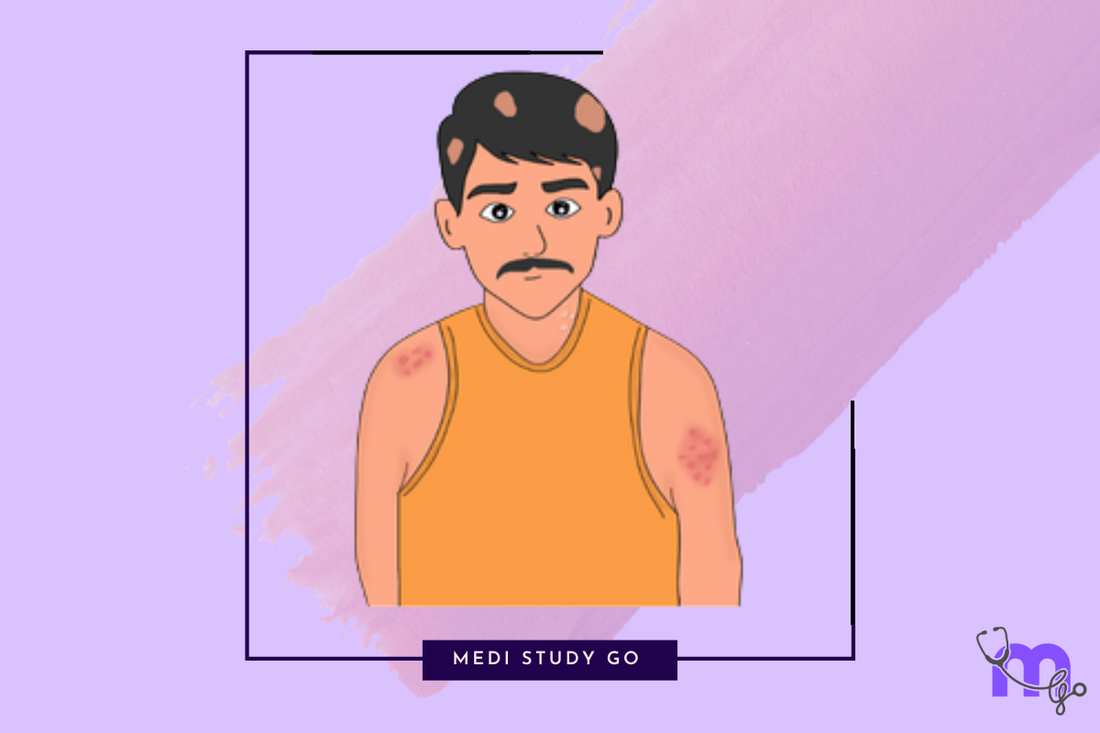
Related resources:
- Understanding Infectious Diseases: A Comprehensive Guide
- Transmission Mechanisms of Infectious Diseases
- Immunity and Host Defense Against Infectious Diseases
- Prevention and Control of Infectious Diseases
- Diagnosis and Management of Infectious Diseases
Introduction
Infectious diseases represent a significant portion of medical practice and feature prominently in medical entrance examinations like NEET. This guide provides detailed information on the pathophysiology and clinical presentations of common infectious diseases, serving as both a revision tool for NEET and a reference for clinical studies.
Bacterial Infections
Enteric Fever (Typhoid and Paratyphoid)
Causative Agent: Salmonella typhi and Salmonella paratyphi A, B, or C
Pathophysiology:
- Ingestion of contaminated food or water introduces the bacteria to the gastrointestinal tract
- Bacteria invade the intestinal mucosa and enter the lymphatics
- They reach mesenteric lymph nodes and eventually enter the bloodstream
- The reticuloendothelial system (liver, spleen, bone marrow) becomes infected
- Bacteria multiply and re-enter the bloodstream, causing secondary bacteremia
- Bacteria infiltrate Peyer's patches in the small intestine
- Secondary bacteremia leads to generalized infection
Clinical Features:
- Incubation period: 5-14 days
- Stepladder pattern of fever (gradually rising and sustained high fever)
- Relative bradycardia (pulse rate slower than expected for the degree of fever)
- Headache, malaise, and myalgia
- Rose spots (salmon-colored macules on the trunk)
- Hepatosplenomegaly
- Abdominal pain and either constipation or diarrhea
- Complications: intestinal perforation, hemorrhage, myocarditis, meningitis

Diphtheria
Causative Agent: Corynebacterium diphtheriae
Pathophysiology:
- The bacteria colonize the upper respiratory tract
- Toxin production (types A and B) is crucial for pathogenesis
- Exotoxin type B helps in binding to cells and facilitates endocytosis
- Exotoxin type A leads to ADP ribosylation of EF-2, inhibiting protein synthesis and causing cell death
- Local tissue damage results in pseudomembrane formation
- Toxin absorption into circulation causes systemic effects
Clinical Features:
- Incubation period: 2-5 days
- Fever, sore throat, malaise
- Thick, gray, adherent pseudomembrane on tonsils, pharynx, or larynx
- "Bull neck" appearance due to cervical lymphadenopathy
- Laryngeal involvement can lead to respiratory obstruction
- Cutaneous diphtheria can occur in some cases
- Complications: myocarditis, polyneuropathy, respiratory failure

Leprosy (Hansen's Disease)
Causative Agent: Mycobacterium leprae
Pathophysiology:
- Bacteria enter through nasal mucosa or skin
- They invade nerves (particularly Schwann cells) and skin
- Clinical manifestations depend on host immune response
- Strong cell-mediated immune response leads to tuberculoid leprosy (TT)
- Weak cell-mediated response leads to lepromatous leprosy (LL)
- Borderline forms (BT, BB, BL) show intermediate immune responses
Clinical Features:
- Incubation period: 2-7 years
- Hypopigmented patches with loss of sensation (especially in tuberculoid form)
- Peripheral nerve thickening (ulnar, posterior tibial, facial nerves commonly affected)
- Skin lesions can be single or multiple depending on the type
- Autonomic dysfunction leading to anhidrosis, temperature dysregulation
- Leonine facies in lepromatous leprosy
- Complications: deformities, blindness, secondary infections

Viral Infections
Measles (Rubeola)
Causative Agent: Measles virus (Morbillivirus)
Pathophysiology:
- Virus enters via respiratory route
- Primary replication in respiratory epithelium and local lymph nodes
- Primary viremia spreads virus to reticuloendothelial system
- Secondary viremia disseminates virus to multiple organs including skin
- Virus suppresses immune system, predisposing to secondary bacterial infections
Clinical Features:
- Incubation period: 6-21 days
- Prodromal phase with the "3 Cs": cough, coryza, conjunctivitis
- Koplik spots (pathognomonic): bluish-white spots on buccal mucosa
- Maculopapular rash starting behind ears and hairline, spreading downward
- Fever, which may spike with rash appearance
- Infectious period: 4 days before to 4 days after rash onset
- Complications: pneumonia, otitis media, encephalitis, post-measles encephalomyelitis
Mumps
Causative Agent: Mumps virus (Paramyxovirus)
Pathophysiology:
- Virus enters via respiratory route
- Replication occurs in upper respiratory epithelium
- Infection of mononuclear cells in regional lymph nodes leads to viremia
- Virus targets epithelial cells of various glands, particularly the parotid gland
- Viral replication causes inflammation and swelling of affected tissues
Clinical Features:
- Incubation period: 16-18 days
- Fever, headache, malaise as prodromal symptoms
- Parotitis (parotid gland swelling) - often bilateral but can be asymmetric
- Pain with chewing or swallowing
- Complications: meningitis, orchitis in males (can cause sterility), oophoritis in females, pancreatitis

Herpes Zoster (Shingles)
Causative Agent: Varicella-zoster virus (HHV-3)
Pathophysiology:
- Primary infection causes chickenpox (varicella)
- Virus establishes latency in dorsal root ganglia or cranial nerve ganglia
- Reactivation occurs years later due to decreased immunity (aging, stress, immunosuppression)
- Virus travels along sensory nerves to the skin in the corresponding dermatome
- Local inflammation and nerve damage cause pain and vesicular eruption
Clinical Features:
- Prodromal phase: pain, burning, or tingling in the affected dermatome
- Unilateral vesicular rash following a dermatome distribution
- Common locations: thoracic dermatomes, trigeminal nerve distribution
- Special forms: herpes zoster ophthalmicus (ophthalmic division of trigeminal nerve), herpes zoster oticus (geniculate ganglion)
- Complications: post-herpetic neuralgia, secondary bacterial infection, scarring, vision loss (in ophthalmicus)

Protozoal Infections
Malaria
Causative Agent: Plasmodium species (P. falciparum, P. vivax, P. ovale, P. malariae, P. knowlesi)
Pathophysiology:
- Female Anopheles mosquito injects Plasmodium sporozoites during blood meal
- Sporozoites infect liver cells and develop into schizonts
- Schizonts rupture, releasing thousands of merozoites
- Merozoites invade red blood cells (RBCs)
- Asexual reproduction within RBCs forms gametocytes
- Periodic rupture of infected RBCs releases toxins and causes fever
- Some parasites develop into male and female gametocytes
- Mosquito ingests gametocytes during blood meal, completing the cycle
Clinical Features:
- Incubation period varies by species (P. falciparum: 12 days)
- Classic paroxysms of fever, chills, and sweating
- Anemia due to RBC destruction
- Hepatosplenomegaly
- Headache, myalgia, fatigue
- Complications of P. falciparum: cerebral malaria, algid malaria, severe anemia, hemoglobinuria, acute respiratory distress syndrome
- P. vivax and P. ovale can cause relapses due to hepatic hypnozoites


Spirochetal Infections
Syphilis
Causative Agent: Treponema pallidum
Pathophysiology:
- Spirochetes enter through mucous membranes or skin abrasions
- Local multiplication leads to primary lesion
- Lymphatic and hematogenous spread occurs early
- Immune response partially controls infection but doesn't eliminate it
- Periods of latency alternate with active disease
Clinical Features:
-
Primary stage (3-90 days after infection):
- Painless, indurated chancre at inoculation site
- Regional lymphadenopathy
- Spontaneously heals in 4-6 weeks
-
Secondary stage (4-10 weeks after infection):
- Disseminated skin rash (including palms and soles)
- Condylomata lata (moist, flat-topped papules in warm areas)
- Generalized lymphadenopathy
- Mucosal lesions, alopecia
- Constitutional symptoms: fever, malaise
-
Latent stage:
- Asymptomatic
- Positive serological tests
- Can last for years
-
Tertiary stage (3-25 years after infection):
- Gummas (chronic granulomatous lesions)
- Cardiovascular syphilis (aortitis, aortic aneurysm)
- Neurosyphilis (tabes dorsalis, general paresis)
-
Congenital syphilis:
- Early manifestations: hepatosplenomegaly, snuffles, rash
- Late manifestations: Hutchinson's teeth, saddle nose, saber shins


Clinical Relevance for NEET Examinations
Understanding the pathophysiology and clinical features of infectious diseases is crucial for NEET and other medical entrance examinations. Some key points to remember:
- Pattern recognition: Learn to recognize classic presentations (e.g., stepladder fever in typhoid, Koplik spots in measles)
- Complications: Know the common and serious complications of each disease
- Differential diagnoses: Understand how to distinguish between infectious diseases with similar presentations
- Special populations: Be familiar with how presentations may differ in children, pregnant women, and immunocompromised patients
-
Examination favorites: Pay special attention to topics frequently tested in NEET, such as:
- Falciparum malaria complications
- Leprosy classification and reactions
- Stages of syphilis
- Diphtheria toxin mechanism
- Measles complications
Practice Questions
- A 25-year-old man presents with fever for 10 days that has gradually increased, relative bradycardia, and rose spots on his trunk. The most likely diagnosis is: a) Leptospirosis b) Enteric fever c) Malaria d) Dengue fever
- A 5-year-old unvaccinated child presents with fever, coryza, conjunctivitis, and bluish-white spots on the buccal mucosa. The diagnosis is: a) Rubella b) Roseola infantum c) Measles d) Scarlet fever
- The most severe form of malaria is caused by: a) Plasmodium vivax b) Plasmodium ovale c) Plasmodium falciparum d) Plasmodium malariae
Conclusion
A thorough understanding of common infectious diseases, their pathophysiology, and clinical presentations is essential for success in medical examinations and future clinical practice. This guide covers key infectious diseases that frequently appear on the NEET and provides a foundation for more detailed study.
For more comprehensive preparation, explore our other resources on infectious diseases, including transmission mechanisms, immunity, prevention strategies, and management approaches.