Hemophilia: Essential Guide for Dental Professionals
Medi Study Go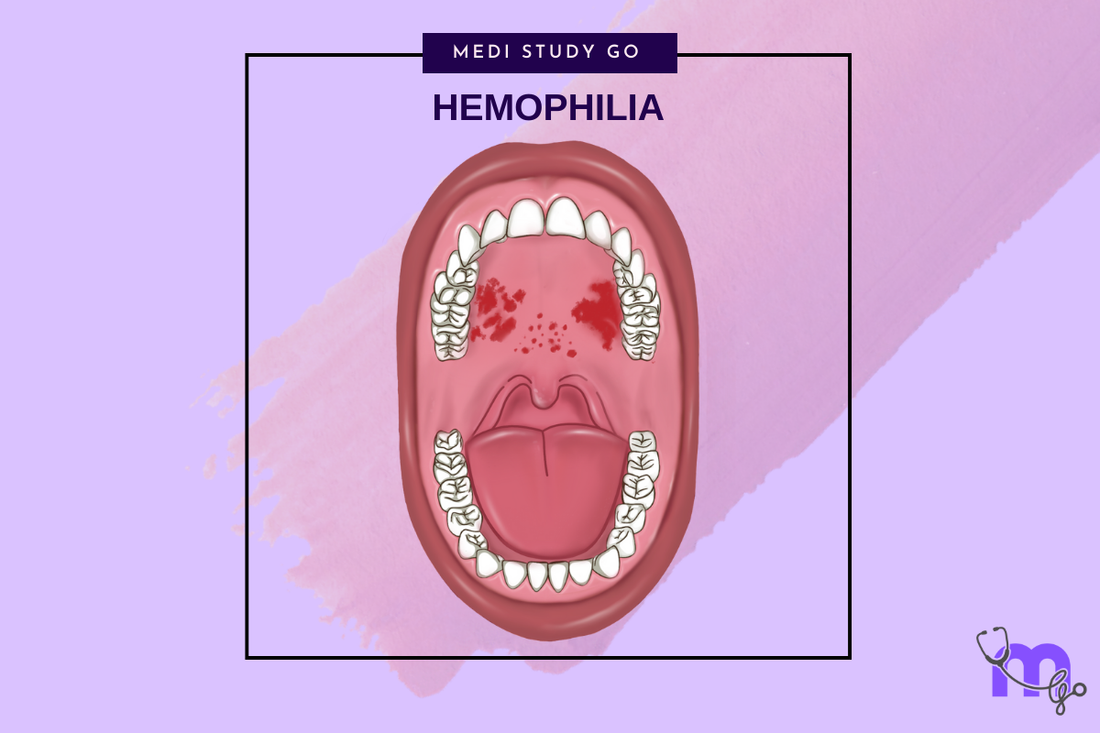
Related resources:
- Oral Manifestations of Hemophilia
- Dental Management Protocols
- Hemophilia Treatment Approaches
- Managing Complications
- Preventive Strategies
Introduction to Hemophilia and Dental Considerations
Hemophilia is a group of inherited bleeding disorders characterized by deficiencies in specific clotting factors that significantly impact dental management. As dental professionals, understanding this genetic disease is crucial for providing safe and effective care to affected patients. This comprehensive guide explores the fundamentals of hemophilia, its oral manifestations, dental management considerations, treatment approaches, and potential complications.
What is Hemophilia?

Understanding the Basics
Hemophilia is a rare X-linked recessive disorder primarily affecting males, though females can be carriers and may exhibit mild symptoms. This bleeding disorder occurs in approximately 1 in 10,000 births, with hemophilia A (factor VIII deficiency) representing about 80% of cases, followed by hemophilia B (factor IX deficiency) at roughly 20%. The condition results from mutations in genes coding for essential clotting factors, leading to inadequate blood coagulation.
The severity of hemophilia disease is classified based on the percentage of functional clotting factor present:
- Severe: <1% of normal factor activity
- Moderate: 1-5% of normal factor activity
- Mild: 5-40% of normal factor activity
This classification directly influences dental management strategies and bleeding risk assessment. Dental professionals preparing for the NEET exam should pay particular attention to these classifications as they frequently appear in NEET previous year question papers.
Pathophysiology and Clinical Presentation
To define hemophilia in physiological terms, it's a condition where the intrinsic pathway of the coagulation cascade is compromised. Without adequate clotting factor function, even minor trauma can lead to prolonged bleeding. The causes of hemophilia are predominantly genetic, with approximately 30% of cases resulting from spontaneous mutations without family history.
The clinical presentation varies widely based on severity but may include:
- Easy bruising
- Prolonged bleeding after injuries, surgeries, or dental procedures
- Spontaneous bleeding into joints (hemarthrosis)
- Spontaneous muscle hematomas
- Intracranial bleeding (severe cases)
For dental professionals, understanding these systemic manifestations provides context for the oral complications that may present in clinical practice. Many NEET preparation books cover these aspects, making them essential study material for the NEET MDS examination.
Oral Manifestations of Hemophilia
The oral cavity can display several characteristic signs of hemophilia that dental professionals should recognize. These manifestations may serve as indicators of undiagnosed hemophilia or reflect inadequate management of known cases.
Gingival Manifestations
Patients with hemophilia commonly experience severe gingival bleeding, particularly during routine dental hygiene procedures or following minor trauma. This bleeding is typically disproportionate to the triggering event and may be difficult to control with conventional measures. Hemosiderin deposits, which appear as brownish discoloration of gingival tissues, may result from recurrent bleeding episodes.
Oral Mucosal Presentations
The oral mucosa in hemophilia patients frequently exhibits:
- Petechiae: Small, pinpoint hemorrhagic spots on the palate, buccal mucosa, or floor of mouth
- Ecchymosis: Larger areas of mucosal bleeding, appearing as bruise-like discolorations
- Hematomas: Localized collections of extravasated blood, which may present on the tongue, lips, or palate
Hard Tissue Considerations
Dental hard tissues may show evidence of hemosiderin deposition, resulting in brownish discoloration of teeth. Additionally, the formation of pseudotumors—subperiosteal hematomas with reactive bone formation—represents a rare but significant finding in the maxillofacial region of hemophilia patients.
Dental Management of Hemophilia Patients
Providing dental care to patients with hemophilia requires careful planning, interdisciplinary communication, and specialized protocols to minimize bleeding risk. This section outlines key considerations for various dental procedures.
Pretreatment Assessment and Planning
Before any dental intervention, comprehensive evaluation is essential:
- Consultation with the patient's hematologist to determine:
- Current factor levels
- History of inhibitor development
- Recommended prophylactic measures
- Laboratory testing to assess:
- Factor activity levels
- Complete blood count
- Activated partial thromboplastin time (aPTT)
- Inhibitor screening if indicated
Local Anesthetic Considerations
The administration of local anesthesia in hemophilia patients requires specific precautions:
- Infiltration techniques and intraligamentary injections generally do not require factor replacement
- Inferior alveolar nerve blocks carry higher bleeding risk and may require factor replacement therapy
- Avoid intramuscular injections when possible
- Consider alternative pain control methods when appropriate
Hemostatic Strategies for Dental Procedures
Various local measures can enhance hemostasis during and after dental procedures:
- Antifibrinolytic agents (e.g., tranexamic acid) in combination with factor replacement therapy
- Application of hemostatic pads to bleeding sites
- Topical thrombin application in direct contact with bleeding areas
- Thrombin and cryoprecipitate patches for persistent bleeding
- Electrocautery and lasers for postoperative hemostasis
For detailed protocols on managing bleeding in dental settings, consult our comprehensive article on Current Treatment Approaches for Hemophilia
Understanding current hemophilia treatment options is essential for coordinating dental care with the patient's overall management plan.
Factor Replacement Therapy
The cornerstone of hemophilia management is factor replacement therapy, which can be administered:
- On-demand: For acute bleeding episodes or before invasive procedures
- Prophylactically: Regular infusions to maintain minimum factor levels and prevent spontaneous bleeding
For dental procedures, factor concentrate infusion is typically recommended one hour before treatment to raise clotting factor levels to the appropriate threshold based on the invasiveness of the planned procedure.
Local Hemostatic Agents
In addition to systemic factor replacement, local hemostatic measures play a critical role in dental management:
- Antifibrinolytic medications (e.g., tranexamic acid, epsilon-aminocaproic acid)
- Fibrin sealants
- Collagen or gelatin-based hemostatic agents
- Oxidized cellulose products
Emerging Therapies and Their Dental Implications
Recent advances in hemophilia treatment include:
- Extended half-life factor products
- Non-factor therapies that mimic factor VIII activity
- Gene therapy approaches
Potential Complications and Their Management
Dental professionals should be aware of potential complications that may arise when treating hemophilia patients and be prepared to manage them effectively.
Inhibitor Development
Approximately 20-30% of severe hemophilia A patients develop antibodies (inhibitors) against factor VIII, complicating treatment and increasing bleeding risk. Dental management of patients with inhibitors requires specialized protocols, potentially including:
- Bypassing agents (activated prothrombin complex concentrates or recombinant factor VIIa)
- Enhanced local hemostatic measures
- Minimally invasive techniques whenever possible
Medication Interference
Certain medications commonly prescribed in dentistry may interfere with hemostasis:
- NSAIDs should be avoided due to platelet function impairment
- Some antibiotics may affect factor metabolism
- Antifungal agents may interact with hemophilia medications
Severe Complications
Rare but serious complications in the dental setting include:
- Fatal airway obstruction due to bleeding in the glottis, particularly following dental anesthesia
- Extensive hematoma formation leading to airway compromise
- Uncontrolled bleeding despite conventional measures
Early recognition and immediate intervention are essential for preventing these life-threatening situations.
Preventive Strategies and Long-term Management
Prevention remains the cornerstone of dental care for hemophilia patients. Comprehensive preventive strategies include:
Maintaining Optimal Oral Hygiene
Patients with hemophilia should be educated on modified oral hygiene techniques that minimize gingival trauma while maintaining effective plaque control. Regular professional cleanings using gentle techniques can help prevent periodontal disease and reduce the need for more invasive treatments.
Preventing Periodontal Disease
Periodontal health is particularly important for hemophilia patients, as periodontal disease can lead to:
- Chronic gingival bleeding
- Tooth mobility
- Increased risk of extractions
- Overall heightened bleeding risk
Regular maintenance using ultrasonic cleaning and laser-assisted scaling with appropriate factor coverage can help manage periodontal conditions while minimizing bleeding complications.
Caries Prevention
A high caries index may necessitate more invasive dental procedures, increasing bleeding risk. Preventive measures should include:
- Regular fluoride applications
- Dietary counseling
- Pit and fissure sealants
- Early intervention for incipient lesions
Conclusion and Future Directions
Dental management of patients with hemophilia requires a multidisciplinary approach, specialized knowledge, and careful planning. By understanding the pathophysiology, recognizing oral manifestations, implementing appropriate precautions, and maintaining excellent preventive care, dental professionals can provide safe and effective treatment for this patient population.
Advances in hemophilia treatment continue to improve quality of life and simplify medical management, with implications for dental care protocols. Staying informed about these developments through NEET revision tools and flashcard applications for NEET will help dental professionals provide optimal care based on current best practices.
For dental students preparing for NEET MDS or other examinations, understanding hemophilia management represents an important clinical competency that frequently appears in NEET q papers. Utilizing flashcard techniques for study and participating in NEET mock tests can help reinforce this knowledge.
By leveraging the comprehensive information provided in this pillar page and the linked detailed resources, dental professionals can develop the expertise needed to confidently manage patients with hemophilia in various clinical scenarios.