Epilepsy: A Comprehensive Guide for Dental and Medical Professionals
Medi Study Go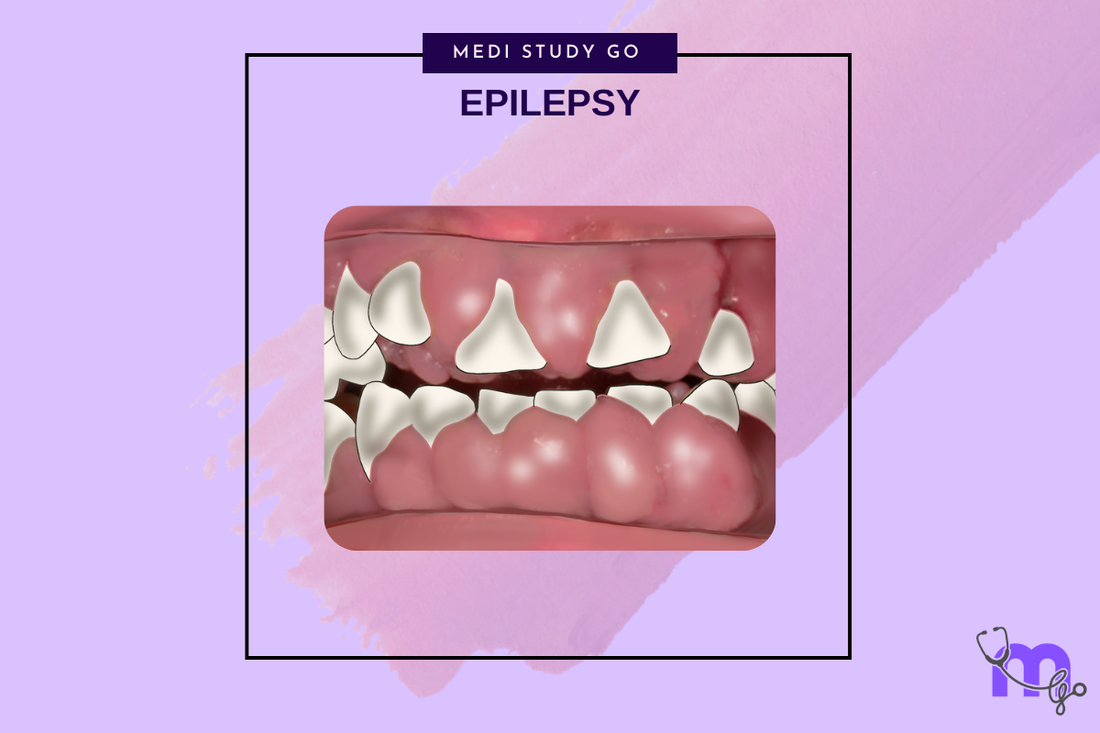
Related resources:
- Dental Management of Epilepsy
- Oral Manifestations
- Treatment Approaches
- Complications
- NEET Exam Guide
Introduction
Epilepsy is one of the most common neurological disorders worldwide, affecting approximately 50 million people globally. For dental and medical professionals, understanding what is epilepsy and its implications is crucial for providing safe and effective patient care. Epilepsy meaning extends beyond just seizures—it represents a complex condition with significant impacts on overall health, including oral health.
As healthcare professionals, particularly those in dentistry, encountering patients with epilepsy requires specialized knowledge and preparation. This comprehensive guide explores the definition, oral manifestations, dental management considerations, treatment approaches, and complications associated with epilepsy, serving as an essential resource for students preparing for medical entrance exams like NEET and practicing clinicians alike.
The relationship between epilepsy and oral health is bidirectional—seizures can impact oral structures, while certain dental procedures may trigger seizures in susceptible individuals. This interconnection necessitates a thorough understanding of epilepsy symptoms, management protocols, and precautionary measures in dental settings.
Understanding Epilepsy
Definition and Diagnostic Criteria
Epilepsy definition encompasses a neurological disorder characterized by recurrent, unprovoked seizures. According to the International League Against Epilepsy (ILAE), the diagnosis of epilepsy requires at least two unprovoked seizures occurring more than 24 hours apart. These seizures result from abnormal, excessive, or synchronous neuronal activity in the brain.
Understanding what causes epilepsy involves recognizing various etiologies:
- Genetic factors
- Congenital abnormalities
- Brain trauma
- Infections affecting the central nervous system
- Stroke
- Brain tumors
- Neurodegenerative diseases
- Metabolic disorders
- Unknown causes (idiopathic epilepsy)
Classification of Epilepsy
The ILAE 2017 classification system categorizes epilepsy into several types:
- Focal epilepsy: Seizures originating in one hemisphere of the brain
- Generalized epilepsy: Seizures involving both hemispheres
- Combined generalized and focal epilepsy: Patients experiencing both types
- Unknown epilepsy: Seizures that cannot be clearly categorized
Seizures associated with epilepsy can present with diverse clinical manifestations including motor and non-motor symptoms. Motor features affecting the head and neck region may include:
- Automatisms (unconscious movements)
- Atonic seizures (sudden loss of muscle tone)
- Clonic movements (rhythmic jerking)
- Spasms (sudden flexion)
- Headaches
For dental professionals, recognizing these manifestations is essential for identifying potential seizure activity during treatment.
Oral Manifestations of Epilepsy
Patients with epilepsy often present with distinctive oral findings that can be attributed to both the condition itself and its treatment. Understanding these manifestations is crucial for comprehensive patient management.
Direct Seizure-Related Oral Manifestations
Seizure activity, particularly in poorly controlled epilepsy, can lead to:
- Dental trauma from falls or convulsions
- Soft tissue injuries including tongue biting
- Temporomandibular joint disorders
- Fractured teeth and soft tissue lacerations
Medication-Induced Oral Manifestations
Antiepileptic drugs (AEDs) are associated with various oral side effects:
- Phenytoin-induced gingival enlargement: A significant complication affecting the anterior labial surfaces of maxillary and mandibular gingivae, typically developing within 2-18 months after medication initiation. This overgrowth can significantly impact oral hygiene, aesthetics, and function.
- Xerostomia and glossitis: Many AEDs reduce salivary flow, leading to dry mouth and inflammation of the tongue. This condition increases the risk of dental caries and oral candidiasis.
- Stomatitis: Mucosal inflammation may occur as an adverse reaction to antiepileptic medications.
- Other oral findings: Intraoral lesions resembling lupus, lip enlargement, and ulcerations can result from long-term AED use.
The frequency and severity of these manifestations vary depending on medication type, dosage, duration, and individual susceptibility. Regular dental examinations are essential for early detection and management of these conditions.
Dental Management of Epilepsy Patients
Pre-Treatment Evaluation
Before initiating dental treatment for patients with epilepsy, a comprehensive evaluation is essential:
- Assess seizure stability: Determine the type, etiology, and frequency of seizures, known triggers, presence of aura, and history of seizure-related injuries.
- Medical consultation: Collaboration with the patient's physician or neurologist is recommended, especially for patients with poorly controlled seizures.
- Laboratory evaluation: Complete blood count with differential, white blood cell and platelet counts, and coagulation studies may be necessary, as AEDs can induce bone marrow suppression and affect clotting.
- Medication review: Evaluate current AED regimen, including serum blood levels, to ensure therapeutic doses are maintained.
Treatment Planning Considerations
Dental treatment for epilepsy patients should be tailored based on seizure control:
- Well-controlled epilepsy: Routine dental care can generally be provided in an outpatient setting with standard protocols.
- Poorly/uncontrolled seizures: Referral to a hospital setting is recommended, as these patients are not suited for conventional outpatient dental care.
- Treatment timing: Schedule appointments during periods when seizures are less likely to occur, typically in the morning when stress and fatigue are minimal.
- Environment modifications: Minimize potential triggers such as bright or flickering lights, and ensure a calm, stress-free environment.
Minimizing Risk During Dental Treatment
Several precautionary measures can reduce risks during dental procedures:
- Use dental floss-secured mouth props: These prevent accidental aspiration or swallowing during seizure activity.
- Implement rubber dam isolation: This provides additional protection during restorative procedures.
- Prefer fixed over removable prostheses: This reduces aspiration risk during potential seizure activity.
- Local anesthetic considerations: No contraindications exist when used in appropriate amounts, though caution is advised with certain AEDs.
- Sedation: May be beneficial for patients with stress-induced seizures or poorly controlled epilepsy, but requires neurologist consultation.
Emergency Management of Seizures
All dental professionals should be prepared to manage seizure emergencies:
- Recognize prodromal signs: These may include unusual sensations, visual disturbances, or behavioral changes.
- Immediate action: Remove dental instruments, clear the area, and position the patient to prevent injury.
- Never force objects between the teeth during a seizure.
- Monitor vital signs and be prepared to administer oxygen if necessary.
- Activate emergency medical services for prolonged seizures (>5 minutes) or repeated seizures without recovery.
Epilepsy Treatment Approaches
Understanding current treatment approaches for epilepsy allows dental professionals to better coordinate care and anticipate potential oral complications.
Pharmacological Management
Antiepileptic drugs (AEDs) remain the cornerstone of epilepsy treatment:
- First-generation AEDs:
- Phenytoin: Commonly associated with gingival overgrowth
- Carbamazepine: May cause insufficient seizure control at low doses or hepatotoxicity at excessive doses
- Sodium valproate: Alternative with fewer oral side effects
- Ethosuximide: Used primarily for absence seizures
- Newer AEDs:
- Lamotrigine
- Levetiracetam
- Topiramate
- Gabapentin
- Pregabalin
These medications generally have fewer oral side effects but may still impact dental care through drug interactions and systemic effects.
Surgical Interventions
For patients with drug-resistant epilepsy, surgical options may include:
- Resection of epileptogenic foci
- Corpus callosotomy
- Vagal nerve stimulation
- Deep brain stimulation
Dental professionals should note that patients with vagal nerve stimulators do not require antibiotic prophylaxis before invasive dental procedures.
Emerging Therapies
Newer approaches to epilepsy management include:
- Responsive neurostimulation
- Dietary therapies (ketogenic diet)
- Cannabidiol-based treatments
These evolving treatments may present unique considerations for oral health management that dental professionals should monitor through continuing education.
Complications of Epilepsy and Antiepileptic Drugs
Blood Dyscrasias
AEDs can induce bone marrow suppression, resulting in:
- Leukopenia
- Thrombocytopenia
- Platelet dysfunction
These hematological alterations increase infection risk, delay healing, and may cause gingival and postoperative bleeding. Dental professionals should:
- Avoid aspirin and NSAIDs in patients taking valproic acid
- Be aware of enhanced bleeding risk with certain medications
- Consider coagulation studies before surgical dental procedures
Oral Complications
Beyond gingival overgrowth, long-term AED use can lead to:
- Increased risk of dental caries due to reduced salivary flow
- Oral candidiasis requiring antifungal management
- Stomatitis and ulcerations requiring symptomatic treatment
- Intraoral lesions resembling lupus erythematosus
Management Strategies
Preventive approaches for epilepsy-related oral complications include:
- Frequent professional dental cleanings
- Electric toothbrush use
- Chlorhexidine and/or folic acid rinses to minimize inflammation
- Topical fluoride applications for caries prevention
- Surgical reduction of significant gingival overgrowth when necessary
Drug Interactions
Dental professionals should be aware of potential interactions between commonly prescribed dental medications and AEDs:
- Macrolide antibiotics may increase carbamazepine levels
- Metronidazole can increase phenytoin and carbamazepine levels
- NSAIDs may displace protein-bound AEDs, increasing free drug concentration
Clinical Considerations for NEET and Medical Students
For students preparing for NEET and other medical entrance examinations, epilepsy represents an important topic with frequent appearance in question papers.
High-Yield Topics for NEET Examination
- ILAE Classification System (2017)
- Pharmacology of antiepileptic drugs
- Management of status epilepticus
- Differential diagnosis of seizure disorders
- Oral manifestations of AEDs
- Emergency management of seizures
Revision Strategies
Effective NEET preparation for epilepsy topics includes:
- Utilizing flashcard techniques for study
- Taking NEET mock tests focusing on neurological disorders
- Reviewing NEET previous year question papers for pattern recognition
- Implementing last minute revision tactics for key concepts
For comprehensive preparation, consider using dedicated revision tools for NEET that incorporate clinical scenarios and application-based questions.
Conclusion
Epilepsy presents unique challenges and considerations for dental and medical professionals. A thorough understanding of the condition—from its definition and classification to its oral manifestations and management protocols—is essential for providing safe, effective care.
The interrelationship between epilepsy, its treatment, and oral health emphasizes the importance of an interdisciplinary approach. By recognizing the various oral manifestations, implementing appropriate management strategies, and staying informed about treatment advances, healthcare professionals can significantly improve outcomes for patients with epilepsy.
For students preparing for NEET and other medical entrance examinations, mastering the concepts outlined in this guide will provide a solid foundation for both academic success and future clinical practice. Remember that while epilepsy remains a challenging condition, appropriate knowledge and preparation enable healthcare providers to deliver optimal care while minimizing risks.